Hyperaldosteronism refers to high levels of aldosterone. Conn’s syndrome refers to an adrenal adenoma producing too much aldosterone.
Hyperaldosteronism may be present in 5-10% of patients with hypertension. Hypertension is the key presenting feature, and many patients are otherwise asymptomatic. It may cause non-specific symptoms such as headaches, muscle weakness and fatigue.
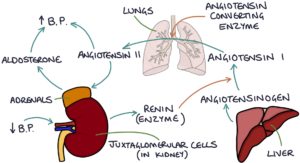
The Renin-Angiotensin-Aldosterone System
Renin is an enzyme by the juxtaglomerular cells in the afferent arterioles in the kidney (there are also some in the efferent arterioles). They sense the blood pressure in these vessels. They secrete more renin in response to low blood pressure and less renin in response to high blood pressure. Renin converts angiotensinogen (released by the liver) into angiotensin I.
Angiotensin I converts to angiotensin II in the lungs with the help of an enzyme called angiotensin-converting enzyme (ACE). Angiotensin II stimulates the release of aldosterone from the adrenal glands.
Aldosterone is a mineralocorticoid steroid hormone. It acts on the nephrons in the kidneys to:
- Increase sodium reabsorption from the distal tubule
- Increase potassium secretion from the distal tubule
- Increase hydrogen secretion from the collecting ducts
Primary Hyperaldosteronism
Primary hyperaldosteronism is when the adrenal glands are directly responsible for producing too much aldosterone. Serum renin will be low as the high blood pressure suppresses it.
The adrenals may produce too much aldosterone for several possible reasons:
- Bilateral adrenal hyperplasia (most common)
- An adrenal adenoma secreting aldosterone (known as Conn’s syndrome)
- Familial hyperaldosteronism (rare)
Secondary Hyperaldosteronism
Secondary hyperaldosteronism is caused by excessive renin stimulating the release of excessive aldosterone.
Excessive renin is released due to disproportionately lower blood pressure in the kidneys, usually due to:
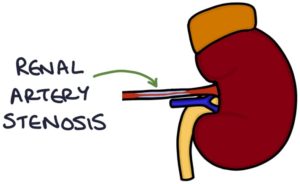
- Renal artery stenosis
- Heart failure
- Liver cirrhosis and ascites
Renal artery stenosis refers to a narrowing of the artery supplying the kidney, usually due to atherosclerosis, similar to the narrowing of the coronary arteries in angina. Renal artery stenosis can be confirmed with:
- Doppler ultrasound
- CT angiogram
- Magnetic resonance angiography (MRA)
Investigations
The aldosterone-to-renin ratio (ARR) is used as a screening test:
- High aldosterone and low renin indicate primary hyperaldosteronism
- High aldosterone and high renin indicate secondary hyperaldosteronism
Other investigations that relate to the effects of aldosterone include:
- Raised blood pressure (hypertension)
- Low potassium (hypokalaemia)
- Blood gas analysis (alkalosis)
Investigations for the underlying cause include:
- CT or MRI to look for an adrenal tumour or adrenal hyperplasia
- Renal artery imaging for renal artery stenosis (Doppler, CT angiogram or MR angiography)
- Adrenal vein sampling of blood from both adrenal veins to locate which gland is producing more aldosterone
Management
Medical management is with aldosterone antagonists:
- Eplerenone
- Spironolactone
Treating the underlying cause involves:
- Surgical removal of the adrenal adenoma
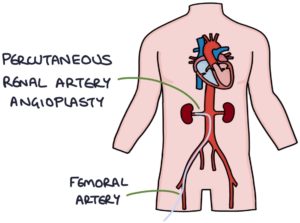
- Percutaneous renal artery angioplasty via the femoral artery to treat renal artery stenosis
TOM TIP: Hyperaldosteronism is worth remembering as the most common cause of secondary hypertension. Consider testing for hyperaldosteronism in patients with hypertension, who are younger, fail to respond to treatment or have a low potassium. Be aware that potassium levels may be normal in hyperaldosteronism.
Updated March 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.