Cushing’s syndrome refers to the features of prolonged high levels of glucocorticoids in the body. There are two groups of corticosteroid hormones:
- Glucocorticoids (e.g., cortisol)
- Mineralocorticoids (e.g., aldosterone)
Cortisol is the primary natural glucocorticoid hormone produced by the adrenal glands.
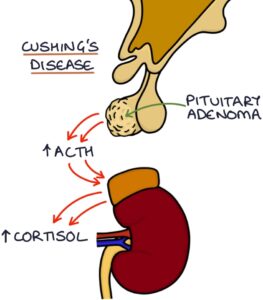
Cushing’s disease refers to a pituitary adenoma secreting excessive adrenocorticotropic hormone (ACTH), which stimulates excessive cortisol release from the adrenal glands. This is not the only cause of Cushing’s syndrome.
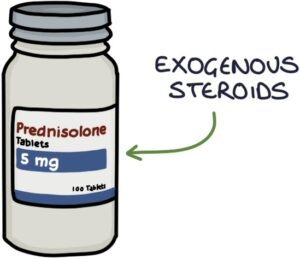
The prolonged use of exogenous corticosteroids (e.g., prednisolone or dexamethasone), often causes Cushing’s syndrome. Exogenous refers to when it originates (-genous) outside (exo-) the body.
Features
Cushing’s features on inspection (round in the middle with thin limbs):
- Round face (known as a “moon face”)
- Central obesity
- Abdominal striae (stretch marks)
- Enlarged fat pad on the upper back (known as a “buffalo hump”)
- Proximal limb muscle wasting (with difficulty standing from a sitting position without using their arms)
- Male pattern facial hair in women (hirsutism)
- Easy bruising and poor skin healing
- Hyperpigmentation of the skin in patients with Cushing’s disease (due to high ACTH levels)
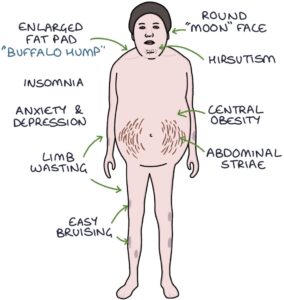
Additional effects include:
- Hypertension
- Cardiac hypertrophy
- Type 2 diabetes
- Dyslipidaemia (raised cholesterol and triglycerides)
- Osteoporosis
- Adverse mental health (e.g., anxiety, depression, insomnia and rarely psychosis)

Causes of Cushing’s Syndrome
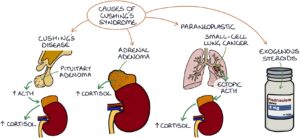
You can remember the causes of Cushing’s syndrome with the “CAPE” mnemonic:
- C – Cushing’s disease (a pituitary adenoma releasing excessive ACTH)
- A – Adrenal adenoma (an adrenal tumour secreting excess cortisol)
- P – Paraneoplastic syndrome
- E – Exogenous steroids (patients taking long-term corticosteroids)
Paraneoplastic Cushing’s syndrome occurs when ACTH is released from a tumour somewhere other than the pituitary gland (ectopic ACTH), stimulating excessive cortisol release. Small-cell lung cancer is the most common.
TOM TIP: A high level of ACTH causes skin pigmentation by stimulating melanocytes in the skin to produce melanin, similar to melanocyte-stimulating hormone. This is an important sign of Cushing’s disease (where excess ACTH comes from a pituitary adenoma) and also primary adrenal insufficiency (where there is inadequate cortisol from the adrenals with a lack of negative feedback to the pituitary). In a patient with Cushing’s syndrome, the pigmentation allows you to determine the cause as excess ACTH, either from Cushing’s disease or ectopic ACTH. This sign is absent in an adrenal adenoma or exogenous steroids.
Dexamethasone Suppression Tests
The dexamethasone suppression tests are used to diagnose Cushing’s syndrome caused by a problem inside the body. There is no point in using them to diagnose Cushing’s syndrome caused by exogenous steroids.
A normal response to dexamethasone is suppressed cortisol due to negative feedback. Dexamethasone causes negative feedback on the hypothalamus, reducing the corticotropin-releasing hormone (CRH) output. It causes negative feedback on the pituitary, reducing the ACTH output. The lower CRH and ACTH levels result in a low cortisol output by the adrenal glands. A lack of cortisol suppression in response to dexamethasone suggests Cushing’s syndrome.
There are three types of dexamethasone suppression test:
- Low-dose overnight test (used as a screening test to exclude Cushing’s syndrome)
- Low-dose 48-hour test (used in suspected Cushing’s syndrome)
- High-dose 48-hour test (used to determine the cause in patients with confirmed Cushing’s syndrome)
For the low-dose overnight test, dexamethasone (1mg) is given at night (usually 10 or 11 pm), and the cortisol is checked at 9 am the following morning. A normal result is that the cortisol level is suppressed. Failure of the dexamethasone to suppress the morning cortisol could indicate Cushing’s syndrome, and further assessment is required.
For the low-dose 48-hour test, dexamethasone (0.5mg) is taken every 6 hours for 8 doses, starting at 9 am on the first day. Cortisol is checked at 9 am on day 1 (before the first dose) and 9 am on day 3 (after the last dose). A normal result is that the cortisol level on day 3 is suppressed. Failure of the dexamethasone to suppress the day 3 cortisol could indicate Cushing’s syndrome, and further assessment is required.
The high-dose 48-hour test is carried out the same way as the low-dose test, other than using 2mg per dose (rather than 0.5mg). This higher dose is enough to suppress the cortisol in Cushing’s syndrome caused by a pituitary adenoma (Cushing’s disease), but not when it is caused by an adrenal adenoma or ectopic ACTH.
Adrenocorticotropic hormone (ACTH) can be measured directly. ACTH is suppressed due to negative feedback on the pituitary when excess cortisol comes from an adrenal tumour (or endogenous steroids). It is high when produced by a pituitary tumour or ectopic ACTH (e.g., small cell lung cancer).
|
Low Dose Test (Cortisol Result) |
High Dose Test (Cortisol Result) |
ACTH |
|
|
Normal |
Low |
Low |
Normal |
|
Adrenal Adenoma |
Not Suppressed |
Not Suppressed |
Low |
|
Pituitary Adenoma |
Not Suppressed |
Low |
High |
|
Ectopic ACTH |
Not Suppressed |
Not Suppressed |
High |
Other Investigations
A 24-hour urinary free cortisol is an alternative to the dexamethasone suppression test. However, it is cumbersome to carry out and does not indicate the underlying cause.
Other investigations:
- Full blood count may show a high white blood cell count
- U&Es may show low potassium if an adrenal adenoma is also secreting aldosterone
- MRI brain for a pituitary adenoma
- CT chest for small cell lung cancer
- CT abdomen for adrenal tumours
Treatment
The primary treatment is to remove the underlying cause:
- Trans-sphenoidal (through the nose) removal of pituitary adenoma
- Surgical removal of adrenal tumour
- Surgical removal of the tumour producing ectopic ACTH (e.g., small cell lung cancer), if possible
Where surgical removal of the cause is not possible, another option is to surgically remove both adrenal glands (adrenalectomy) and give the patient life-long steroid replacement therapy.
Nelson’s syndrome involves the development of an ACTH-producing pituitary tumour after the surgical removal of both adrenal glands due to a lack of cortisol and negative feedback. It causes skin pigmentation (high ACTH), bitemporal hemianopia and a lack of other pituitary hormones.
Metyrapone reduces the production of cortisol in the adrenals and is occasionally used in treating of Cushing’s.
Last updated March 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.