Adrenal insufficiency is where the adrenal glands do not produce enough steroid hormones, particularly cortisol and aldosterone. Steroids are essential for life. Therefore, the condition is life-threatening unless the hormones are replaced.
Physiology
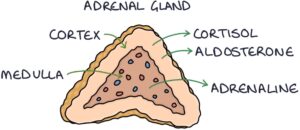
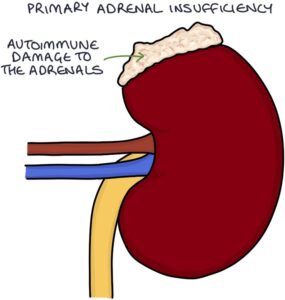
There are two adrenal glands, found in the abdomen. The adrenal glands sit on top of the kidneys. The outer part of the adrenal gland is called the cortex and the inner part is called the medulla.
The adrenal cortex produces two types of steroid hormones:
- Cortisol (a glucocorticoid)
- Aldosterone (Mineralocorticoid)
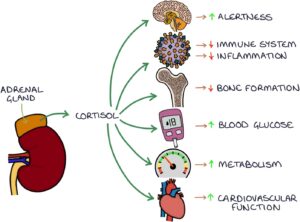
Glucocorticoids (e.g., cortisol) help the body cope with stress, increase the blood glucose level, regulate the immune system and reduce inflammation.
Mineralocorticoids (e.g., aldosterone) help regulate the balance of electrolytes and blood pressure. They act on the nephrons in the kidneys to:
- Increase sodium reabsorption from the urine to the blood in the distal tubule
- Increase potassium secretion from the blood to the urine in the distal tubule
- Increase hydrogen secretion from the blood to the urine in the collecting ducts
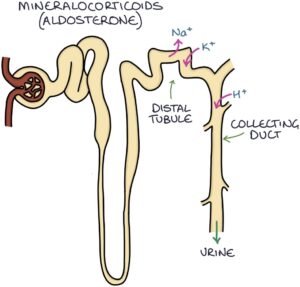
When sodium is reabsorbed in the kidneys, water follows it by osmosis. This leads to increased intravascular volume (the volume of fluid inside blood vessels), increasing the blood pressure.
Hypothalamic-Pituitary-Adrenal Axis
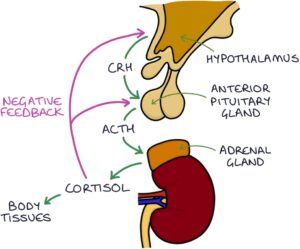
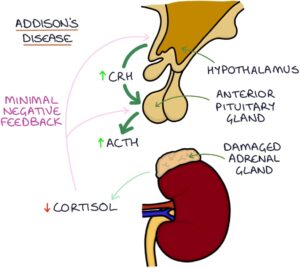
Cortisol is controlled by two structures in the brain called the hypothalamus and the pituitary gland, specifically the anterior part of the pituitary. This is called the hypothalamic-pituitary-adrenal (HPA) axis.
The hypothalamus releases corticotropin-releasing hormone (CRH). CRH stimulates the anterior pituitary to release adrenocorticotropic hormone (ACTH). ACTH stimulates the adrenal glands to release cortisol.
Cortisol travels to the body tissues to carry out its effects. It also travels to the brain and has a suppressing effect on the hypothalamus and the pituitary. This is called negative feedback. Too much cortisol suppresses the release of CRH and ACTH, helping to keep cortisol levels within normal limits.
When the cortisol level gets too high, it suppresses the secretion of CRH and ACTH. Lower CRH and ACTH result in less adrenal gland stimulation and less cortisol secretion, returning the cortisol levels to normal.
Causes of Adrenal Insufficiency
Addison’s disease refers specifically to when the adrenal glands have been damaged, resulting in reduced cortisol and aldosterone secretion. This is called primary adrenal insufficiency. The most common cause is autoimmune.
In primary adrenal insufficiency, the low cortisol means reduced negative feedback on the hypothalamus and pituitary, leading to increased CRH and ACTH.
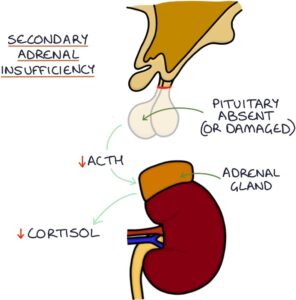
Secondary adrenal insufficiency results from inadequate adrenocorticotropic hormone (ACTH) and a lack of stimulation of the adrenal glands, leading to low cortisol. This is the result of loss or damage to the pituitary gland. Secondary adrenal insufficiency can be due to:
- Tumours (e.g., pituitary adenomas)
- Surgery to the pituitary
- Radiotherapy
- Sheehan’s syndrome (where major post-partum haemorrhage causes avascular necrosis of the pituitary gland)
- Trauma
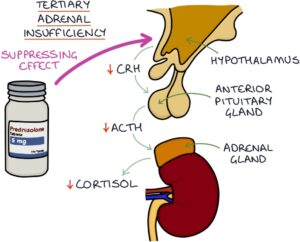
Tertiary adrenal insufficiency results from inadequate corticotropin-releasing hormone (CRH) release by the hypothalamus. This is usually the result of patients taking long-term oral steroids (for more than 3 weeks), causing suppression of the hypothalamus (via negative feedback). When the exogenous steroids (originating outside the body) are suddenly withdrawn, the hypothalamus does not “wake up” fast enough, and endogenous steroids (originating inside the body) are not adequately produced. Therefore, long-term steroids must be tapered slowly to allow the adrenal axis to regain normal function.
Presentation
The symptoms of adrenal insufficiency are:
- Fatigue
- Muscle weakness
- Muscle cramps
- Dizziness and fainting
- Thirst and craving salt
- Weight loss
- Abdominal pain
- Depression
- Reduced libido

The signs of adrenal insufficiency are:
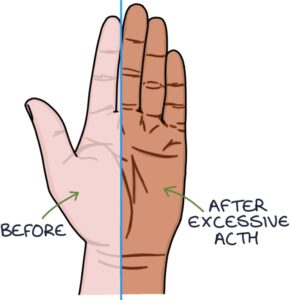
- Bronze hyperpigmentation of the skin, particularly in creases (ACTH stimulates melanocytes to produce melanin)
- Hypotension (particularly postural hypotension – with a drop of more than 20 mmHg on standing)
The bronze hyperpigmentation of the skin is caused by excessive ACTH, stimulating melanocytes to produce melanin. It mainly affects skin creases (e.g., on the palms), scars, lips and buccal mucosa.
TOM TIP: If you see a patient in an OSCE exam who may have adrenal insufficiency, check for a medical alert bracelet worn to alert medical services that they are steroid-dependent if they become unconscious.

Investigations
Hyponatraemia (low sodium) is a key biochemical finding. This may be the only presenting feature.
Other potential biochemical findings may occur. Normal results do not exclude the diagnosis:
- Hyperkalaemia (high potassium)
- Hypoglycaemia (low glucose)
- Raised creatinine and urea due to dehydration
- Hypercalcaemia (high calcium)
Early morning cortisol (8 – 9 am) has a role but is often falsely normal.
The short Synacthen test is the test of choice for diagnosing adrenal insufficiency.
Adrenocorticotropic hormone (ACTH) can be measured directly. The ACTH level is high in primary adrenal insufficiency, as the pituitary is producing lots of ACTH without negative feedback in the absence of cortisol. The ACTH level is low in secondary adrenal failure.
Autoantibodies may be present in autoimmune adrenal insufficiency:
- Adrenal cortex antibodies
- 21-hydroxylase antibodies
CT or MRI of the adrenal glands can be helpful if suspecting structural pathology. They are not routinely required.
MRI of the pituitary gives further information about pituitary pathology.
Short Synacthen Test
The short Synacthen test is also known as the ACTH stimulation test. It is the test of choice for diagnosing adrenal insufficiency. It is ideally performed in the morning.
The test involves giving a dose of Synacthen, which is synthetic ACTH. The blood cortisol is checked before and 30 and 60 minutes after the dose. The synthetic ACTH will stimulate healthy adrenal glands to produce cortisol. The cortisol level should at least double. A failure of cortisol to double indicates either:
- Primary adrenal insufficiency (Addison’s disease)
- Very significant adrenal atrophy after a prolonged absence of ACTH in secondary adrenal insufficiency
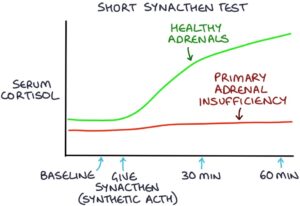
The long Synacthen test was used to distinguish between primary adrenal insufficiency and adrenal atrophy due to secondary adrenal insufficiency. It is rarely used because checking the ACTH level will give the same answer. ACTH is high in primary adrenal insufficiency and low in secondary adrenal insufficiency.
Management
Treatment of adrenal insufficiency is with replacement steroids titrated to signs, symptoms and electrolytes. Hydrocortisone (a glucocorticoid) is used to replace cortisol. Fludrocortisone (a mineralocorticoid) is used to replace aldosterone, if aldosterone is also insufficient.
Patients are given a steroid card, ID tag and emergency letter to alert emergency services that they depend on steroids for life. Doses should not be missed, as they are essential to life. Doses are doubled during an acute illness to match the normal steroid response to illness.
Patients and close contacts are taught to give intramuscular hydrocortisone in an emergency.
Adrenal Crisis
Adrenal crisis, also known as Addisonian crisis, describes an acute presentation of severe adrenal insufficiency, where the absence of steroid hormones leads to a life-threatening emergency. They may present with:
- Reduced consciousness
- Hypotension
- Hypoglycaemia
- Hyponatraemia and hyperkalaemia

It may be the initial presentation of adrenal insufficiency or triggered by infection, trauma or other acute illness in established adrenal insufficiency. Do not wait to perform investigations and establish a definitive diagnosis before starting treatment in suspected adrenal crisis.
Management involves:
- ABCDE approach to initial assessment and arrange transfer to hospital
- Intramuscular or intravenous hydrocortisone (the initial dose is 100mg, followed by an infusion or 6 hourly doses)
- Intravenous fluids
- Correct hypoglycaemia (e.g., IV dextrose)
- Careful monitoring of electrolytes and fluid balance
Last updated March 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

