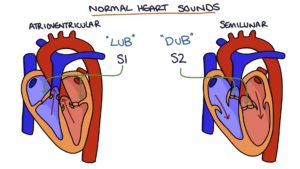
Normal Heart Sounds
The first heart sound (S1) is caused by the closing of the atrioventricular valves (the tricuspid and mitral valves) at the start of the systolic contraction of the ventricles.
The second heart sound (S2) is caused by the closing of the semilunar valves (the pulmonary and aortic valves) once the systolic contraction is complete.
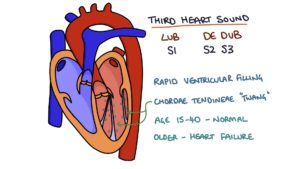
3rd Heart Sound
A third heart sound (S3) is heard roughly 0.1 seconds after the second heart sound. Think of it as rapid ventricular filling causing the chordae tendineae to pull to their full length and twang like a guitar string. The extra heart sound can result in what is described as a “gallop rhythm”.
S3 can be normal in young (15-40 years) healthy people because the heart functions so well that the ventricles allow rapid filling. In older patients, it can indicate heart failure, as the ventricles and chordae are stiff and weak and reach their limit much faster than usual. Think of this like tight hamstrings in an old de-conditioned patient sharply tightening as they bend forward.
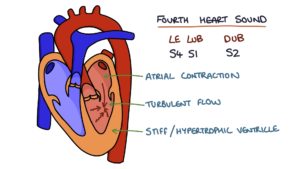
4th Heart Sound
A fourth heart sound (S4) is heard directly before S1. This is always abnormal and relatively rare to hear. It indicates a stiff or hypertrophic ventricle and is caused by turbulent flow from that atria contracting against a non-compliant ventricle.
Listening to Murmurs
Auscultate with the stethoscope bell to better hear low-pitched sounds and the diaphragm to listen to high-pitched sounds. To remember this think of a child’s high-pitched screaming from their diaphragm and a church bell giving a deep “bong”.
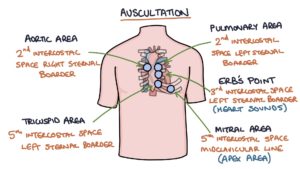
Listen over the 4 valve areas in turn for murmurs:
- Pulmonary area – in the 2nd intercostal space, left sternal border
- Aortic – 2nd intercostal space, right sternal border
- Tricuspid – 5th intercostal space, left sternal border
- Mitral – 5th intercostal space, mid clavicular line (apex area)
Listen to Erb’s point. This is in the third intercostal space on the left sternal border and is the best area for listening to heart sounds (S1 and S2).
Special manoeuvres can be used to emphasise certain murmurs:
- Position the patient on their left side for mitral stenosis
- Position the patient sat up, leaning forward and holding exhalation for aortic regurgitation
Assessing a Murmur
The features of a murmur can be remembered with the “SCRIPT” mnemonic:
- S – Site: where is the murmur loudest?
- C – Character: soft / blowing / crescendo (getting louder) / decrescendo (getting quieter) / crescendo-decrescendo (louder then quieter)
- R – Radiation: can you hear the murmur over the carotids (aortic stenosis) or left axilla (mitral regurgitation)?
- I – Intensity: what grade is the murmur?
- P – Pitch: is it high-pitched or low and rumbling? Pitch indicates velocity.
- T – Timing: is it systolic or diastolic?
Murmur Grade
Grading a murmur is quite subjective. However, it is helpful in assessing the severity of the defect and will help you sound clever when presenting your findings. When in doubt, it is probably grade 2 or 3.
- Grade I: Difficult to hear
- Grade II: Quiet
- Grade III: Easy to hear
- Grade IV: Easy to hear with a palpable thrill
- Grade V: Audible with stethoscope barely touching the chest
- Grade VI: Audible with stethoscope off the chest
Describing a Murmur
You can use this script to describe a murmur in your exams. Use it to describe potential murmurs during your OSCE practice sessions so that it becomes second nature, and you will sound very slick when presenting to the examiner.
“This patient has a harsh / soft / blowing, Grade …, systolic / diastolic murmur, heard loudest in the aortic / mitral / tricuspid / pulmonary area, that does not / radiates to the carotids / left axilla. It is high / low pitched and has a crescendo / decrescendo / crescendo-decrescendo shape. This is suggestive of a diagnosis of mitral stenosis / aortic stenosis.”
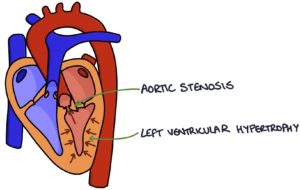
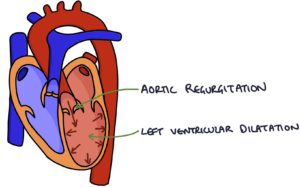
Hypertrophy and Dilatation
Valvular heart disease can cause hypertrophy (thickening both outwards and into the chamber) or dilatation (thinning and expanding, like blowing up a balloon) of the myocardium in different heart areas. This affects the chamber immediately before the pathological valve (e.g., the left ventricle in aortic pathology and the left atrium in mitral pathology).
When pushing against a stenotic valve, the muscle has to try harder, resulting in hypertrophy:
- Mitral stenosis causes left atrial hypertrophy
- Aortic stenosis causes left ventricular hypertrophy
When a leaky valve allows blood to flow back into a chamber, it stretches the muscle, resulting in dilatation:
- Mitral regurgitation causes left atrial dilatation
- Aortic regurgitation causes left ventricular dilatation
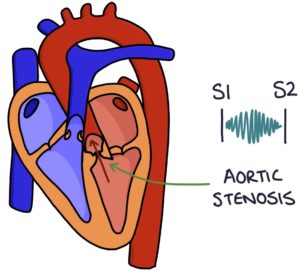
Aortic Stenosis
Aortic stenosis is the most common valvular heart disease and the most common indication for valve replacement surgery. It refers to narrowing of the aortic valve, restricting blood flow from the left ventricle to the aorta.
Aortic stenosis causes an ejection-systolic, high-pitched murmur due to the high blood flow velocity through the aortic valve. This has a crescendo-decrescendo character due to the speed of blood flow across the value during the different periods of systole. Flow during systole is slowest at the start and end and fastest in the middle.
The murmur radiates to the carotids as the turbulence continues into the neck.
Other signs of aortic stenosis:
- Thrill in the aortic area on palpation
- Slow rising pulse
- Narrow pulse pressure (the difference between systolic and diastolic blood pressure)
- Exertional syncope (lightheadedness and fainting when exercising) due to difficulty maintaining a good flow of blood to the brain
Causes of aortic stenosis:
- Idiopathic age-related calcification (by far the most common cause)
- Bicuspid aortic valve
- Rheumatic heart disease
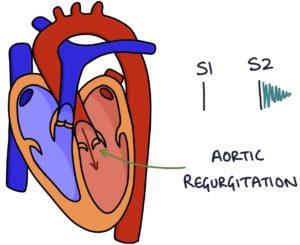
Aortic Regurgitation
Aortic regurgitation refers to an incompetent aortic valve, allowing blood to flow back from the aorta into the left ventricle.
Aortic regurgitation typically causes an early diastolic, soft murmur.
It can also cause an Austin-Flint murmur. This is heard at the apex as a diastolic “rumbling” murmur. This is caused by blood flowing back through the aortic valve and over the mitral valve, causing it to vibrate.
Other signs of aortic regurgitation:
- Thrill in the aortic area on palpation
- Collapsing pulse
- Wide pulse pressure
- Heart failure and pulmonary oedema
A collapsing pulse or water hammer pulse is a forcefully appearing and rapidly disappearing pulse. This is typically felt in the radial artery with the patient’s arm held straight upwards. It occurs as blood is forcefully pumped out of the left ventricle, then immediately flows backwards through the incompetent aortic valve.
Causes of aortic regurgitation:
- Idiopathic age-related weakness
- Bicuspid aortic valve
- Connective tissue disorders, such as Ehlers-Danlos syndrome and Marfan syndrome
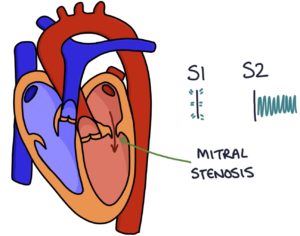
Mitral Stenosis
Mitral stenosis is a narrowed mitral valve restricting blood flow from the left atrium into the left ventricle.
Mitral stenosis causes a mid-diastolic, low-pitched “rumbling” murmur due to a low blood flow velocity. There will be a loud S1 due to thick valves requiring a large systolic force to shut, then shutting suddenly. There is an opening snap after S2, which triggers the onset of the murmur.
Other signs of mitral stenosis:
- Tapping apex beat, which is a palpable, prominent S1
- Malar flush
- Atrial fibrillation (irregularly irregular pulse)
Malar flush refers to red discolouration of the skin over the upper cheeks and nose. It is due to the back pressure of blood into the pulmonary system, causing a rise in CO2 and vasodilation.
Atrial fibrillation is caused by the left atrium struggling to push blood through the stenotic valve causing strain, electrical disruption and resulting fibrillation.
Causes of mitral stenosis:
- Rheumatic heart disease
- Infective endocarditis
TOM TIP: When examining a patient with heart valve pathology, look for signs of the potential underlying cause. For example, look for signs of infective endocarditis in a patient with mitral stenosis, such as splinter haemorrhages, Janeway lesions, Osler’s nodes and splenomegaly, and offer fundoscopy for Roth spots. Look for signs of Marfan syndrome in a patient with aortic regurgitation, such as tall stature, long limbs, arachnodactyly (long slender fingers) and a high-arched palate. This will make you look very clever.
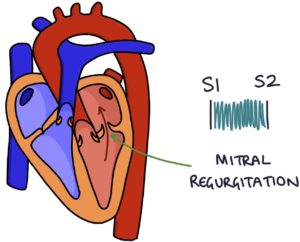
Mitral Regurgitation
Mitral regurgitation refers to an incompetent mitral valve, allowing blood to flow back from the left ventricle to the left atrium during systolic contraction of the left ventricle. The leaking valve causes a reduced ejection fraction and a backlog of blood waiting to be pumped through the left side of the heart, resulting in congestive cardiac failure. Mitral regurgitation is the second most common indication for valve replacement.
Mitral regurgitation causes a pan-systolic, high-pitched “whistling” murmur due to high-velocity blood flow through the leaky valve. The murmur radiates to the left axilla. You may hear a third heart sound.
Other signs of mitral regurgitation:
- Thrill in the mitral area on palpation
- Signs of heart failure and pulmonary oedema
- Atrial fibrillation (irregularly irregular pulse)
Causes of mitral regurgitation:
- Idiopathic weakening of the valve with age
- Ischaemic heart disease
- Infective endocarditis
- Rheumatic heart disease
- Connective tissue disorders, such as Ehlers-Danlos syndrome or Marfan syndrome
Tricuspid Regurgitation
Tricuspid regurgitation refers to an incompetent tricuspid valve, allowing blood to flow back from the right ventricle to the right atrium during systolic contraction of the right ventricle.
Tricuspid regurgitation causes a pan-systolic murmur. There is a split second heart sound due to the pulmonary valve closing earlier than the aortic valve, as the right ventricle empties faster than the left ventricle.
Other signs of tricuspid regurgitation:
- Thrill in the tricuspid area on palpation
- Raised JVP with giant C-V waves (Lancisi’s sign)
- Pulsatile liver (due to regurgitation into the venous system)
- Peripheral oedema
- Ascites
Causes of tricuspid regurgitation:
- Pressure due to left-sided heart failure or pulmonary hypertension (“functional”)
- Infective endocarditis
- Rheumatic heart disease
- Carcinoid syndrome
- Ebstein’s anomaly
- Connective tissue disorders, such as Marfan syndrome
Pulmonary Stenosis
Pulmonary stenosis is a narrowed pulmonary valve, restricting blood flow from the right ventricle into the pulmonary arteries.
Pulmonary stenosis causes an ejection systolic murmur loudest in the pulmonary area with deep inspiration. There is a widely split second heart sound, as the left ventricle empties much faster than the right ventricle.
Other signs of pulmonary stenosis:
- Thrill in the pulmonary area on palpation
- Raised JVP with giant A waves (due to the right atrium contracting against a hypertrophic right ventricle)
- Peripheral oedema
- Ascites
Pulmonary stenosis is usually congenital and may be associated with:
- Noonan syndrome
- Tetralogy of Fallot
Tetralogy of Fallot is a congenital condition where there are four coexisting pathologies:
- Ventricular septal defect (VSD)
- Overriding aorta
- Pulmonary valve stenosis
- Right ventricular hypertrophy
Last updated March 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

