Supraventricular tachycardia (SVT) refers to when abnormal electrical signals from above (supra-) the ventricles cause a fast heart rate (tachycardia).
Pathophysiology
Normally, the electrical signals of the heart start in the sinoatrial node. The sinoatrial node is the heart’s natural pacemaker, dictating when the heart beats. It is located at the junction between the superior vena cava and the right atrium. The electrical signal travels through the right and left atrium, causing the atria to contract. Then it travels through the atrioventricular (AV) node, which is the pathway between the upper part (atria) and lower part (ventricles) of the heart, down to the ventricles, causing the ventricles to contract. The electrical signal in the heart can only go in one direction, from the atria to the ventricles. Normally, electrical activity cannot travel from the ventricles to the atria.
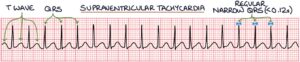
Supraventricular tachycardia is caused by the electrical signal re-entering the atria from the ventricles. The electrical signal finds a way from the ventricles back into the atria. Once the signal is back in the atria, it again travels through the atrioventricular node to the ventricles, causing another ventricular contraction. This causes a self-perpetuating electrical loop without an endpoint, resulting in narrow complex tachycardia. It is described as a “narrow complex”, as the QRS complex has a duration of less than 0.12 seconds.
Paroxysmal SVT describes a situation where SVT reoccurs and remits in the same patient over time.
Narrow Complex Tachycardia
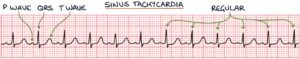
Narrow complex tachycardia is a fast heart rate with a QRS complex duration of less than 0.12 seconds. On a standard 25 mm/sec ECG, 0.12 seconds equals 3 small squares. Therefore, the QRS complex will fit within 3 small squares in SVT. On an ECG, SVT looks like a QRS complex followed immediately by a T wave, QRS complex, T wave and so on.
There are four main differentials of a narrow complex tachycardia. There are key ECG features that will help you differentiate these:
- Sinus tachycardia
- Supraventricular tachycardia
- Atrial fibrillation
- Atrial flutter
Sinus tachycardia will take the normal P wave, QRS complex and T wave pattern. Sinus tachycardia is not an arrhythmia and is usually a response to an underlying cause, such as sepsis or pain.
Atrial fibrillation can be identified on an ECG by:
- Absent P waves
- Narrow QRS complex tachycardia
- Irregularly irregular ventricular rhythm (as opposed to SVT, which causes a regular rhythm)

In atrial flutter, the atrial rate is usually around 300 beats per minute and gives a saw-tooth pattern on the ECG. A QRS complex occurs at regular intervals depending on how often there is conduction from the atria. This often results in two atrial contractions for every one ventricular contraction, giving a ventricular rate of 150 beats per minute.

Supraventricular tachycardia looks like a QRS complex followed immediately by a T wave, then a QRS complex, then a T wave, and so on. There are P waves, but they are often buried in the T waves, so you cannot see them. It can be distinguished from atrial fibrillation by the regular rhythm and atrial flutter by the absence of a saw-tooth pattern.
It can be tricky to distinguish SVT from sinus tachycardia. SVT has an abrupt onset and a very regular pattern without variability. Sinus tachycardia has a more gradual onset and more variability in the rate. The history is also important, where sinus tachycardia usually has an explanation (e.g., pain or fever), while SVT can appear at rest with no apparent cause.
Sometimes it can be difficult to distinguish between the different causes, so always seek help from an experienced person when in doubt.
TOM TIP: SVT can cause a broad complex tachycardia if the patient also has a bundle branch block. Therefore, consider this differential in patients with tachycardia and wide QRS complexes. The most important thing to remember is that SVT causes a narrow complex tachycardia.
Types
There are three main types of SVT, based on the source of the abnormal electrical signal.
Atrioventricular nodal re-entrant tachycardia is where the re-entry point is back through the atrioventricular node. This is the most common type of SVT.
Atrioventricular re-entrant tachycardia is where the re-entry point is an accessory pathway. An additional electrical pathway, somewhere between the atria and the ventricles, lets electricity back through from the ventricles to the atria. Having an extra electrical pathway connecting the atria and ventricles is called Wolff-Parkinson-White syndrome.
Atrial tachycardia is where the electrical signal originates in the atria somewhere other than the sinoatrial node. This is not caused by a signal re-entering from the ventricles but from abnormally generated electrical activity in the atria.
Wolff-Parkinson-White Syndrome
Wolff-Parkinson-White syndrome (WPW) is caused by an extra electrical pathway connecting the atria and ventricles. It is also called pre-excitation syndrome. Normally, only the atrioventricular (AV) node connects the atria and ventricles. The extra pathway in Wolff-Parkinson-White syndrome may be called the Bundle of Kent. The additional pathway allows electrical activity to pass between the atria and ventricles, bypassing the atrioventricular node. This electrical pathway might not cause any symptoms, or it might cause episodes of SVT.
ECG changes in Wolff-Parkinson-White syndrome are:
- Short PR interval, less than 0.12 seconds
- Wide QRS complex, greater than 0.12 seconds
- Delta wave
The delta wave appears as a slurred upstroke in the QRS complex. It is caused by the electricity prematurely entering the ventricles through the accessory pathway.
The definitive treatment for Wolff-Parkinson-White syndrome is radiofrequency ablation of the accessory pathway.
In someone with a combination of atrial fibrillation or atrial flutter and WPW, there is a risk that the chaotic atrial electrical activity can pass through the accessory pathway into the ventricles, causing a polymorphic wide complex tachycardia, which is a life-threatening medical emergency. The heart rate can get above 200, or even 300, beats per minute, and ventricular fibrillation and cardiac arrest can follow. Most anti-arrhythmic medications (e.g., beta blockers, calcium channel blockers, digoxin and adenosine) increase this risk by reducing conduction through the AV node and promoting conduction through the accessory pathway. Therefore, they are contra-indicated in patients with WPW that develop atrial fibrillation or flutter.
Acute Management
Management here summarises the Resuscitation Council UK guidelines (2021) to help with exam preparation. Get experienced senior support and refer to local and national guidelines when managing patients.
The patient should have continuous ECG monitoring during management.
Management of supraventricular tachycardia in patients without life-threatening features involves a stepwise approach, trying each step to see whether it works before moving on.
- Step 1: Vagal manoeuvres
- Step 2: Adenosine
- Step 3: Verapamil or a beta blocker
- Step 4: Synchronised DC cardioversion
Patients with life-threatening features, such as loss of consciousness (syncope), heart muscle ischaemia (e.g., chest pain), shock or severe heart failure, are treated with synchronised DC cardioversion under sedation or general anaesthesia. Intravenous amiodarone is added if initial DC shocks are unsuccessful.
Patients with Wolff-Parkinson-White syndrome (pre-excitation syndrome) with possible atrial arrhythmias (e.g., atrial fibrillation or atrial flutter) should not have adenosine, verapamil or a beta blocker, as these block the atrioventricular node, promoting conduction of the atrial rhythm through the accessory pathway into the ventricles, causing potentially life-threatening ventricular rhythms. Sometimes it can be difficult to distinguish this from SVT, so the involvement of experienced seniors is essential. In this scenario, the usual management is procainamide (which does not block the AV node) or electrical cardioversion (if unstable).
Vagal Manoeuvres
Vagal manoeuvres stimulate the vagus nerve, increasing the activity in the parasympathetic nervous system. This can slow the conduction of electrical activity in the heart, terminating an episode of supraventricular tachycardia.
Valsalva manoeuvres involve increasing the intrathoracic pressure. This can be achieved by having the patient blow hard against resistance, for example, blowing into a 10ml syringe for 10-15 seconds.
Carotid sinus massage involves stimulating the baroreceptors in the carotid sinus by massaging that area on one side of the neck (not both sides at the same time). Carotid sinus massage is avoided in patients with carotid artery stenosis (e.g., with a carotid bruit or previous TIA).
The diving reflex involves briefly submerging that patient’s face in cold water.
Adenosine
Adenosine works by slowing cardiac conduction, primarily through the AV node. It interrupts the AV node or accessory pathway during SVT and “resets” it to sinus rhythm. The half-life of adenosine is less than 10 seconds, meaning it is very quickly metabolised and stops having an effect. It needs to be given as a rapid bolus to ensure it reaches the heart with enough impact to interrupt the pathway for a short period. It will often cause a brief period of asystole or bradycardia that can be scary for the patient and doctor. However, it metabolises quickly, and sinus rhythm will return.
Adenosine is avoided in patients with:
- Asthma
- COPD
- Heart failure
- Heart block
- Severe hypotension
- Potential atrial arrhythmia with underlying pre-excitation
Adenosine must be given as a rapid IV bolus into a large proximal cannula (e.g., grey cannula in the antecubital fossa). The patient should be warned about the scary feeling of dying or impending doom when it is injected. This feeling quickly passes.
Three doses are attempted until sinus rhythm returns:
- Initially 6mg
- Then 12mg
- Then 18mg
Synchronised DC Cardioversion
Synchronised DC (direct current) cardioversion involves an electric shock applied to the heart to restore normal sinus rhythm. A defibrillator machine monitors the electrical signal, particularly identifying the R waves. An electric shock is synchronised with a ventricular contraction, at the R wave on the ECG. If successful, the shock will be followed by sinus rhythm.
Synchronised cardioversion is used in patients with a pulse to avoid shocking the patient during a T wave. Delivering a shock during a T wave can result in ventricular fibrillation and, subsequently, cardiac arrest.
During a cardiac arrest scenario with pulseless ventricular tachycardia or ventricular fibrillation, where the patient does not have organised electrical activity or a pulse, there is no need for the shock to be synchronised.
Management of Paroxysmal SVT
Patients with recurrent episodes of supraventricular tachycardia can be treated to prevent further episodes. The options are:
- Long-term medication (e.g., beta blockers, calcium channel blockers or amiodarone)
- Radiofrequency ablation
Radiofrequency Ablation
Catheter ablation is performed in a catheter laboratory, often called a “cath lab”. It involves a general anaesthetic or sedation. A catheter is inserted into a femoral vein and fed through the venous system under x-ray guidance to the heart.
Once in the heart, the catheter tip is placed against different areas to test the electrical signals. The operator attempts to identify the location of any abnormal electrical pathways. Once identified, radiofrequency ablation (heat) is applied to burn the abnormal electrical pathway. This leaves scar tissue that does not conduct electrical activity. Destroying the abnormal electrical pathway aims to remove the source of the arrhythmia.
Radiofrequency ablation can permanently resolve certain arrhythmias caused by abnormal electrical pathways, including:
- Atrial fibrillation
- Atrial flutter
- Supraventricular tachycardias
- Wolff-Parkinson-White syndrome
Last updated April 2024
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

