Severe pathology of the aortic or mitral valves may be an indication for surgical replacement of that valve. Replacement of the tricuspid valve is very rare.
Aortic stenosis is the most common valvular heart disease and the most common indication for valve replacement surgery. Mitral regurgitation is the second most common indication for valve replacement.
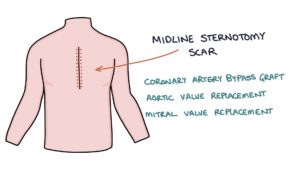
Patients that have had a valve replacement will have a scar. Usually, this will be a midline sternotomy scar straight down the middle of the sternum, indicating a mitral or aortic valve replacement or a coronary artery bypass graft (CABG). Less commonly, a right-sided mini-thoracotomy incision can be used for minimally invasive mitral valve surgery.
Bioprosthetic Versus Mechanical
Valves can be either replaced by a bioprosthetic or a metallic mechanical valve.
Bioprosthetic valves have a limited lifespan of around 10 years. “Porcine” bioprosthetic valves come from a pig.
Mechanical valves have a good lifespan (well over 20 years) but require lifelong anticoagulation with warfarin. The INR target range with mechanical valves is 2.5 – 3.5 (higher than the 2 – 3 target for atrial fibrillation).
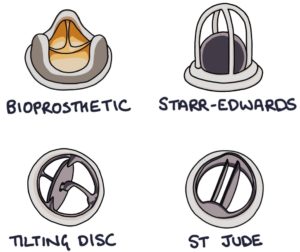
Mechanical Heart Valves
Starr-Edwards valves feature a ball in a cage. The ball moves away from the opening to let blood through, then moves back against the opening to prevent blood from regurgitating through the valve. They were successful but are no longer used due to the high risk of thrombus formation.
Tilting disc valves feature a single tilting disc.
St Jude valves consist of two tilting metal discs. The two discs mean they are called bileaflet valves. Of the three mechanical valves listed, the St Jude valve has the smallest risk of thrombus formation.
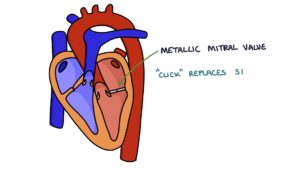
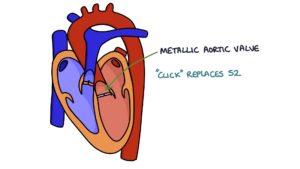
It is possible to hear a click when auscultating the heart sounds in a patient with a mechanical valve:
A click replaces S1 for metallic mitral valves.
A click replaces S2 for metallic aortic valves.
There are three major complications of mechanical heart valves:
- Thrombus formation (blood stagnates and clots)
- Infective endocarditis (infection in the prosthesis)
- Haemolysis causing anaemia (blood gets churned up in the valve)
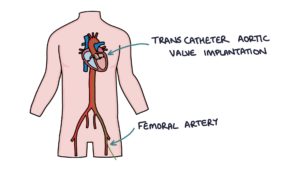
Transcatheter Aortic Valve Implantation
Transcatheter aortic valve implantation (TAVI) is a treatment for severe aortic stenosis, usually in patients at high risk for an open valve replacement operation. It involves local or general anaesthetic, inserting a catheter into the femoral artery, feeding a wire under x-ray guidance to the location of the aortic valve, inflating a balloon to stretch the stenosed aortic valve and implanting a bioprosthetic valve in the location of the aortic valve.
Long-term outcomes for TAVI still need to be clarified as it is a relatively new procedure. Therefore, open surgery is still the first-line option in younger, fitter patients.
Patients with a TAVI do not typically require warfarin as the valve is bioprosthetic.
Infective Endocarditis
Infective endocarditis occurs in around 2.5% of patients having a surgical valve replacement. The rate is slightly lower for TAVI at about 1.5%. Infective endocarditis in a prosthetic valve has quite a high mortality of about 15%. This is usually caused by one of three gram-positive cocci organisms:
- Staphylococcus
- Streptococcus
- Enterococcus
Last updated March 2023
