Pericarditis is inflammation of the pericardium, the membrane surrounding the heart. The most common causes are idiopathic (no underlying cause) and viral. It presents with chest pain and fever and is treated with NSAIDs.
Pathophysiology
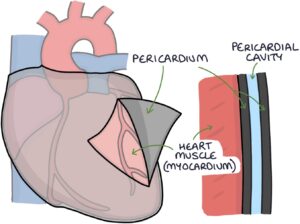
The membrane that surrounds the heart is called the pericardium or pericardial sac. It has two layers with a small amount of fluid in between (less than 50mls), providing lubrication. These layers separate the heart from the rest of the contents of the mediastinum. Lubrication between the two layers allows the heart to beat without generating too much friction.
There is a potential space between the two layers, called the pericardial cavity. The two layers usually touch each other, which is why it is only a potential space.
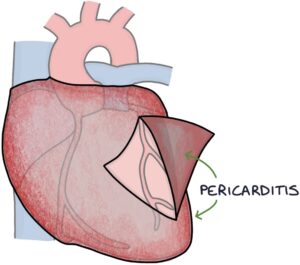
Pericarditis refers to inflammation of the pericardium.
There are many potential underlying causes for the inflammation:
- Idiopathic (no underlying cause)
- Infection (e.g., tuberculosis, HIV, coxsackievirus, Epstein–Barr virus and other viruses)
- Autoimmune and inflammatory conditions (e.g., systemic lupus erythematosus and rheumatoid arthritis)
- Injury to the pericardium (e.g., after myocardial infarction, open heart surgery or trauma)
- Uraemia (raised urea) secondary to renal impairment
- Cancer
- Medications (e.g., methotrexate)
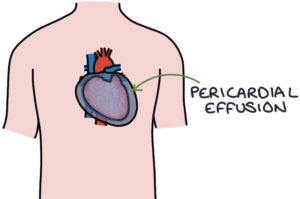
Pericardial effusion is when the potential space of the pericardial cavity fills with fluid. This creates an inward pressure on the heart, making it more difficult to expand during diastole (filling of the heart).
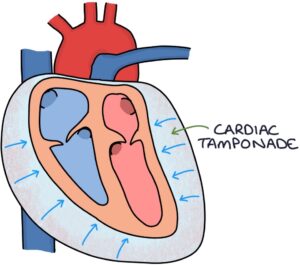
Pericardial tamponade (or cardiac tamponade) is where the pericardial effusion is large enough to raise the intra-pericardial pressure. This increased pressure squeezes the heart and affects its ability to function. It reduces heart filling during diastole, decreasing cardiac output during systole. This is an emergency and requires prompt drainage of the pericardial effusion to relieve the pressure.
Presentation
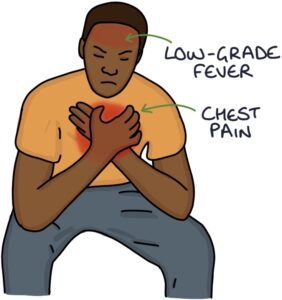
Two key presenting features should make you think of pericarditis:
- Chest pain
- Low-grade fever
The chest pain is:
- Sharp
- Central/anterior
- Worse with inspiration (pleuritic)
- Worse on lying down
- Better on sitting forward
Pericardial friction rub on auscultation is a key examination finding. A pericardial rub is a rubbing, scratching sound that occurs alongside the heart sounds.
Investigations
Blood tests show raised inflammatory markers (white blood cells, CRP and ESR).
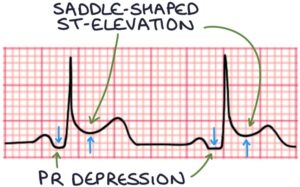
ECG changes include:
- Saddle-shaped ST-elevation
- PR depression
Echocardiogram can be used to diagnose a pericardial effusion.
Management
Management involves:
- Non-steroidal anti-inflammatory drugs (NSAIDs) are the mainstay of treatment (e.g., aspirin or ibuprofen)
- Colchicine (taken longer-term, e.g., 3 months, to reduce the risk of recurrence)
Steroids may be used second-line, in recurrent cases or associated with inflammatory conditions (e.g., rheumatoid arthritis)
Underlying causes, such as tuberculosis and renal failure, should be treated appropriately.
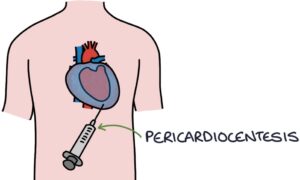
Pericardiocentesis may be required to remove fluid from around the heart if there is a significant pericardial effusion or tamponade.
Most cases resolve within a month. It can be recurrent, returning after previously having resolved. Some cases may persist long-term, called chronic pericarditis.
Last updated March 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

