Acute coronary syndrome (ACS) is usually the result of a thrombus from an atherosclerotic plaque blocking a coronary artery. When a thrombus forms in a fast-flowing artery, it is formed mainly of platelets. This is why antiplatelet medications such as aspirin, clopidogrel and ticagrelor are the mainstay of treatment.
There are three types of acute coronary syndrome:
- Unstable angina
- ST-elevation myocardial infarction (STEMI)
- Non-ST-elevation myocardial infarction (NSTEMI)
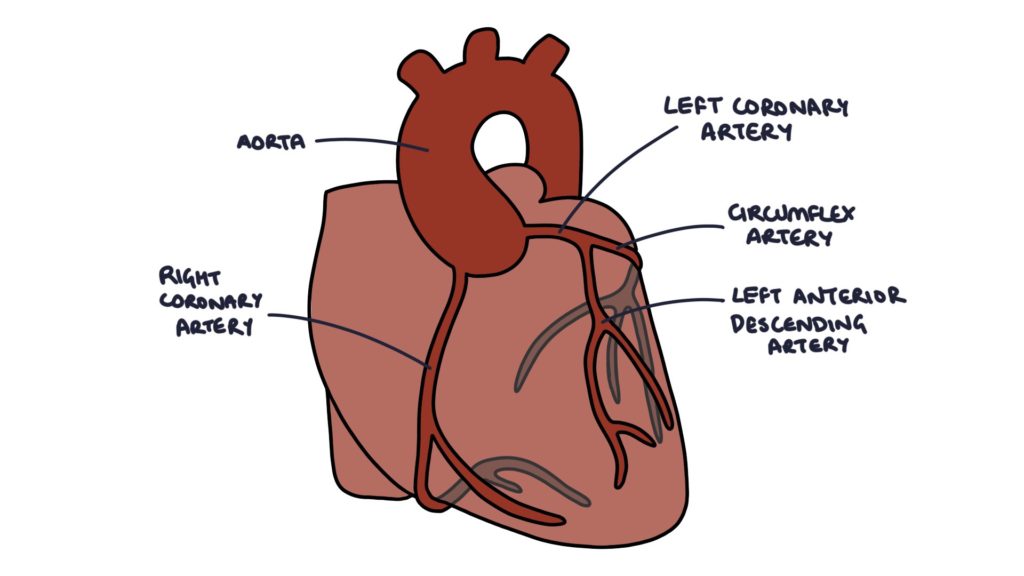
Coronary Artery Anatomy
Two coronary arteries branch from the root of the aorta:
- Right coronary artery (RCA)
- Left coronary artery (LCA)
The right coronary artery (RCA) curves around the right side and under the heart and supplies the:
- Right atrium
- Right ventricle
- Inferior aspect of the left ventricle
- Posterior septal area
The left coronary artery becomes the:
- Circumflex artery
- Left anterior descending (LAD)
The circumflex artery curves around the top, left and back of the heart and supplies the:
- Left atrium
- Posterior aspect of the left ventricle
The left anterior descending (LAD) travels down the middle of the heart and supplies the:
- Anterior aspect of the left ventricle
- Anterior aspect of the septum
Presentation
Acute coronary syndrome typically presents with central, constricting chest pain.
The chest pain is often associated with:
- Pain radiating to the jaw or arms
- Nausea and vomiting
- Sweating and clamminess
- A feeling of impending doom
- Shortness of breath
- Palpitations
Symptoms should continue at rest for more than 15 minutes.
A silent myocardial infarction is when someone does not experience typical chest pain during acute coronary syndrome. Patients with diabetes are particularly at risk of silent MIs.
ECG Changes in Acute Coronary Syndrome
STEMI:
- ST-segment elevation
- New left bundle branch block
NSTEMI:
- ST segment depression
- T wave inversion
Pathological Q waves suggest a deep infarction involving the full thickness of the heart muscle (transmural) and typically appear 6 or more hours after the onset of symptoms.
|
Artery |
Heart Area |
ECG Leads |
|
Left coronary artery |
Anterolateral |
I, aVL, V3-6 |
|
Left anterior descending |
Anterior |
V1-4 |
|
Circumflex |
Lateral |
I, aVL, V5-6 |
|
Right coronary artery |
Inferior |
II, III, aVF |
Troponin
Troponin is a protein in cardiac muscle (myocardium) and skeletal muscle. The specific type of troponin, normal range and diagnostic criteria vary based on different laboratories, so check the local policy. A rise in troponin is consistent with myocardial ischaemia, as they are released from the ischaemic muscle tissue.
Troponin results are used to diagnose an NSTEMI. They are not required to diagnose a STEMI, as this is diagnosed based on the clinical presentation and ECG findings.
Assessment may involve repeated troponin tests, depending on the local policy (e.g., at baseline and 3 hours after the onset of symptoms). A high troponin or a rising troponin on repeat tests, in the context of suspected acute coronary syndrome, indicates an NSTEMI.
Troponin is a non-specific marker, meaning that a raised troponin does not automatically imply acute coronary syndrome. The alternative causes of a raised troponin include:
- Chronic kidney disease
- Sepsis
- Myocarditis
- Aortic dissection
- Pulmonary embolism
Other Investigations
Additional investigations in patients with suspected or confirmed acute coronary syndrome are:
- Baseline bloods, including FBC, U&E, LFT, lipids and glucose
- Chest x-ray to investigate for pulmonary oedema and other causes of chest pain
- Echocardiogram once stable to assess the functional damage to the heart, specifically the left ventricular function
Classification
Patients with acute cardiac-sounding chest pain will have an ECG and troponin blood test as part of their workup. The results of the ECG and troponin will determine the type of acute coronary syndrome.
STEMI is diagnosed when the ECG shows either:
- ST elevation
- New left bundle branch block
NSTEMI is diagnosed when there is a raised troponin, with either:
- A normal ECG
- Other ECG changes (ST depression or T wave inversion)
Unstable angina is diagnosed when there are symptoms suggest ACS, the troponin is normal, and either:
- A normal ECG
- Other ECG changes (ST depression or T wave inversion)
When a patient is presenting with chest pain and the troponin and ECG are normal, the diagnosis is either unstable angina or another cause, such as musculoskeletal chest pain.
Initial Management
The information here is based on the chest pain NICE guidelines (updated 2016) and acute coronary syndrome (updated 2020) and aims to help you with exam preparation. Follow local guidelines and get senior support when managing patients.
In patients presenting with symptoms of acute coronary syndrome, the initial management can be remembered with the “CPAIN” mnemonic:
- C – Call an ambulance
- P – Perform an ECG
- A – Aspirin 300mg
- I – Intravenous morphine for pain if required (with an antiemetic, e.g., metoclopramide)
- N – Nitrate (GTN)
When the patient is pain-free, but the pain occurred within the past 72 hours, they need to be referred to the hospital for same-day assessment, usually to be seen by the medical team in the Ambulatory Care Unit (depending on local pathways). They may require emergency admission if there are ECG changes or complications (e.g., signs of heart failure).
Management of STEMI
Patients with STEMI presenting within 12 hours of onset should be discussed urgently with the local cardiac centre for either:
- Percutaneous coronary intervention (PCI) (if available within 2 hours of presenting)
- Thrombolysis (if PCI is not available within 2 hours)
The cardiac centre will advise about medications to be given in preparation for PCI, such as aspirin and prasugrel.
Percutaneous coronary intervention (PCI) involves putting a catheter into the patient’s radial or femoral artery (radial is preferred), feeding it up to the coronary arteries under x-ray guidance and injecting contrast to identify the area of blockage (angiography). Blockages can be treated using balloons to widen the lumen (angioplasty) or devices to remove or aspirate the blockage. Usually, a stent is inserted to keep the artery open.
Thrombolysis involves injecting a fibrinolytic agent. Fibrinolytic agents work by breaking down fibrin in blood clots. There is a significant risk of bleeding, which can make thrombolysis dangerous. Some examples of thrombolytic agents are streptokinase, alteplase and tenecteplase.
Management of NSTEMI
The medical management of an NSTEMI can be remembered with the “BATMAN” mnemonic:
- B – Base the decision about angiography and PCI on the GRACE score
- A – Aspirin 300mg stat dose
- T – Ticagrelor 180mg stat dose (clopidogrel if high bleeding risk, or prasugrel if having angiography)
- M – Morphine titrated to control pain
- A – Antithrombin therapy with fondaparinux (unless high bleeding risk or immediate angiography)
- N – Nitrate (GTN)
Give oxygen only if their saturation drops (less than 95% in someone without COPD).
Angiography in NSTEMI
Unstable patients are considered for immediate angiography, similar to with a STEMI.
The GRACE score gives a 6-month probability of death after having an NSTEMI.
- 3% or less is considered low risk
- Above 3% is considered medium to high risk
Patients at medium or high risk are considered for early angiography with PCI (within 72 hours).
Ongoing Management
After the initial management, patients require:
- Echocardiogram once stable to assess the functional damage to the heart, specifically the left ventricular function
- Cardiac rehabilitation
- Secondary prevention
Medication for secondary prevention can be remembered with the “6 A’s” mnemonic:
- Aspirin 75mg once daily indefinitely
- Another Antiplatelet (e.g., ticagrelor or clopidogrel) for 12 months
- Atorvastatin 80mg once daily
- ACE inhibitors (e.g. ramipril) titrated as high as tolerated
- Atenolol (or another beta blocker – usually bisoprolol) titrated as high as tolerated
- Aldosterone antagonist for those with clinical heart failure (i.e. eplerenone titrated to 50mg once daily)
Dual antiplatelet therapy will vary following PCI procedures, depending on the type of stent that was inserted.
It is particularly essential to closely monitor the renal function in patients taking ACE inhibitors and aldosterone antagonists. Both can cause hyperkalaemia (raised potassium). The MHRA issued a safety update in 2016 that using spironolactone or eplerenone (aldosterone antagonists) plus an ACE inhibitor or angiotensin receptor blocker carries a risk of fatal hyperkalaemia.
Complications
The complications of a myocardial infarction can be remembered with the “DREAD” mnemonic:
- D – Death
- R – Rupture of the heart septum or papillary muscles
- E – “oEdema” (heart failure)
- A – Arrhythmia and Aneurysm
- D – Dressler’s Syndrome
Dressler’s Syndrome
Dressler’s syndrome is also called post-myocardial infarction syndrome. It usually occurs around 2 – 3 weeks after an acute myocardial infarction. It is caused by a localised immune response that results in inflammation of the pericardium, the membrane that surrounds the heart (pericarditis). It has become less common as the management of acute coronary syndrome has advanced.
It presents with pleuritic chest pain, low-grade fever and a pericardial rub on auscultation. A pericardial rub is a rubbing, scratching sound that occurs alongside the heart sounds. It can cause a pericardial effusion and rarely a pericardial tamponade (where the fluid constricts the heart and inhibits function).
A diagnosis can be made with an ECG (global ST elevation and T wave inversion), echocardiogram (pericardial effusion) and raised inflammatory markers (CRP and ESR).
Management is with NSAIDs (e.g., aspirin or ibuprofen) and, in more severe cases, steroids (e.g., prednisolone). Pericardiocentesis may be required to remove fluid from around the heart, if there is a significant pericardial effusion.
Types of Myocardial Infarction
Knowing the types of myocardial infarction is helpful for exams. These terms are not frequently used in everyday practice as they may be confusing for those that are not familiar with them.
- Type 1: Traditional MI due to an acute coronary event
- Type 2: Ischaemia secondary to increased demand or reduced supply of oxygen (e.g. secondary to severe anaemia, tachycardia or hypotension)
- Type 3: Sudden cardiac death or cardiac arrest suggestive of an ischaemic event
- Type 4: MI associated with procedures such as PCI, coronary stenting and CABG
You could remember these with the “ACDC” mnemonic:
- Type 1: A – ACS-type MI
- Type 2: C – Can’t cope MI
- Type 3: D – Dead by MI
- Type 4: C – Caused by us MI
Last updated March 2023
