Trochanteric bursitis refers to inflammation of a bursa over the greater trochanter on the outer hip.
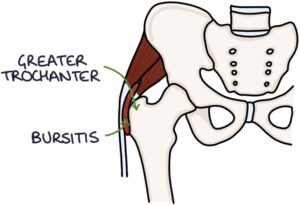
It produces pain localised at the outer hip, referred to as greater trochanteric pain syndrome.
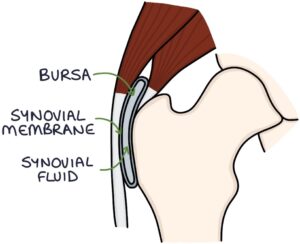
Bursae are sacs created by synovial membrane filled with a small amount of synovial fluid. They are found at bony prominences (e.g., at the greater trochanter, knee, shoulder and elbow). They act to reduce friction between the bones and soft tissues during movement.
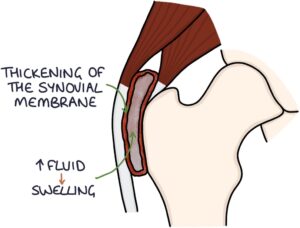
Bursitis refers to inflammation of a bursa. This causes thickening of the synovial membrane and increased fluid production, causing swelling.
This inflammation can have several causes:
- Friction from repetitive movements
- Trauma
- Inflammatory conditions (e.g., rheumatoid arthritis)
- Infection – referred to as septic bursitis
Presentation
The typical presentation is a middle-aged patient with gradual-onset lateral hip pain (over the greater trochanter) that may radiate down the outer thigh. The pain is described as aching or burning. It is worse with activity, standing after sitting for a prolonged period and trying to sit cross-legged. It may disrupt sleep and be difficult to find a comfortable lying position.
On examination, there is tenderness over the greater trochanter. There is not usually any swelling (unlikely bursitis in other areas).
The NICE clinical knowledge summaries (updated 2016) suggest special tests to establish the diagnosis:
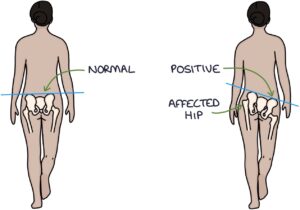
- Trendelenburg test
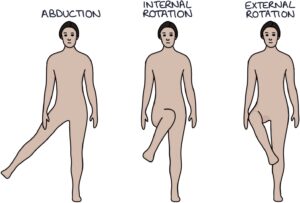
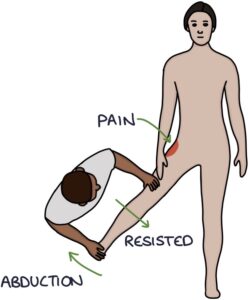
- Resisted abduction of the hip
- Resisted internal rotation of the hip
- Resisted external rotation of the hip
The Trendelenburg test involves asking the patient to stand one-legged on the affected leg. Normally, the other side of the pelvis should remain level or tilt upwards slightly. A positive Trendelenburg test is when the other side of the pelvis drops down, suggesting weakness in the affected hip.
To perform the resisted movements, ask the patient to resist while you move their hip. For example, with the patient lying supine, abduct their leg at the hip while they try to resist the movement. This causes the soft tissues associated with the bursa to tighten, causing pain. Pain on resisted movement supports a diagnosis of bursitis.
Management
The diagnosis is based on the history and examination findings.
Management options are:
- Rest
- Ice
- Analgesia (e.g., ibuprofen or naproxen)
- Physiotherapy
- Steroid injections
Rarely, trochanteric bursitis can be caused by infection. This may present with warmth, erythema, swelling and pain over the bursa. The patient may have a fever. Treatment involves antibiotics.
It can take 6-9 months to recover fully, sometimes longer.
Last updated August 2021
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

