Leukoplakia
Leukoplakia is characterised by white patches in the mouth, often on the tongue or insides of the cheeks (buccal mucosa). It is a precancerous condition, meaning it increases the risk of squamous cell carcinoma of the mouth.
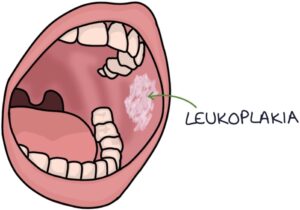
The patches are asymptomatic, irregular and slightly raised. They are fixed in place, meaning they cannot be scraped off.
They may require a biopsy to exclude abnormal cells (dysplasia) or cancer. Management involves stopping smoking, reducing alcohol intake, close monitoring and potentially laser removal or surgical excision.
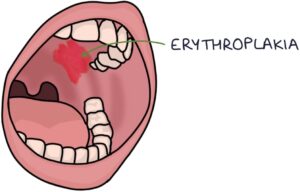
Erythroplakia
Erythroplakia is similar to leukoplakia, except the lesions are red. Erythroleukoplakia refers to lesions that are a mixture of red and white. Both erythroplakia and erythroleukoplakia are associated with a high risk of squamous cell carcinoma and should be referred urgently to exclude cancer.
Lichen Planus
Lichen planus is an autoimmune condition that causes localised chronic inflammation of the skin. The skin has shiny, purplish, flat-topped raised areas with white lines across the surface called Wickham’s striae. It usually occurs in patients over 45 and is more common in women.
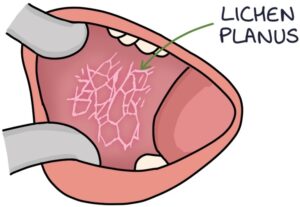
Lichen planus can also affect the mucosal membranes, including the mouth. Often it only affects the mouth.
In the mouth, it can take three patterns:
- Reticular
- Erosive
- Plaque
A reticular pattern involves a net-like web of white lines called Wickham’s striae.
Erosive lesions are where the surface layer of the mucosa is eroded, leaving bright red and sore areas of mucosa.
Plaques are larger continuous areas of white mucosa.
Management involves good oral hygiene, stopping smoking and topical steroids.
Gingivitis
Gingivitis refers to inflammation of the gums. This can present with swollen gums, bleeding after brushing, painful gums and bad breath (halitosis). Gingivitis can lead to periodontitis if not adequately managed.

Periodontitis refers to severe and chronic inflammation of the gums and the tissues that support the teeth. This often leads to loss of teeth.
Acute necrotising ulcerative gingivitis is a rapid onset of more severe inflammation in the gums. It presents similarly to gingivitis, however, it is painful. Anaerobic bacteria usually cause this.
The risk factors for gingivitis are:
- Plaque build-up on the teeth (inadequate brushing)
- Smoking
- Diabetes
- Malnutrition
- Stress
Bacteria live in plaque, damaging the teeth and gums. Hardened plaque is called tartar.
Patients with gingivitis will be managed by a dentist. Treatment involves:
- Good oral hygiene
- Stopping smoking
- Dental hygienist treatment to remove plaque and tartar
- Chlorhexidine mouth wash
- Antibiotics for acute necrotising ulcerative gingivitis (e.g., metronidazole)
- Dental surgery if required
Gingival Hyperplasia
Gingival hyperplasia refers to abnormal growth of the gums. The gums are notably enlarged around the teeth.
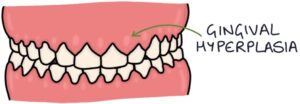
Possible causes of gingival hyperplasia include:
- Gingivitis
- Pregnancy
- Vitamin C deficiency (scurvy)
- Acute myeloid leukaemia
- Medications, particularly calcium channel blockers, phenytoin and ciclosporin
Aphthous Ulcers
Aphthous ulcers are very common, small, painful ulcers of the mucosa in the mouth. They have a well-circumscribed, punched-out, white appearance.
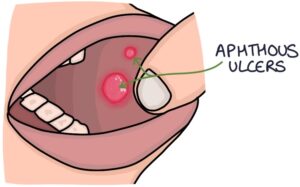
Aphthous ulcers commonly occur in otherwise healthy people, with no underlying cause. They may be triggered by emotional or physical stress, trauma to the mucosa or particular foods.
They may also be an indication of underlying conditions, notably:
- Inflammatory bowel disease (Crohn’s disease and ulcerative colitis)
- Coeliac disease
- Behçet disease
- Vitamin deficiency (e.g., iron, B12, folate and vitamin D)
- HIV
Aphthous ulcers usually heal within 2 weeks. Manageable ulcers do not require any intervention.
Topical treatments can be used to treat symptoms, including:
- Choline salicylate (e.g., Bonjela)
- Benzydamine (e.g., Difflam spray)
- Lidocaine
Topical corticosteroids can be used in more severe ulcers. These may reduce the duration and severity of symptoms. Options include:
- Hydrocortisone buccal tablets applied to the lesion
- Betamethasone soluble tablets applied to the lesion
- Beclomethasone inhaler sprayed directly onto the lesion
The NICE guidelines on suspected cancer (updated January 2021) recommend a two week wait referral in patients with “unexplained ulceration” lasting over 3 weeks.
Last updated July 2021
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

