Venous thromboembolism (VTE) is a common and potentially fatal condition. It involves a blood clot (thrombus) developing in the circulation, usually secondary to blood stagnation or hypercoagulable states. When a thrombus develops in a deep vein, it is called a deep vein thrombosis (DVT).
Once a thrombus has developed, it can travel (embolise) from the deep veins, through the right side of the heart and into the lungs, where it becomes lodged in the pulmonary arteries. This blocks blood flow to areas of the lungs and is called a pulmonary embolism (PE).
If the patient has a septal defect in their heart (e.g., an atrial septal defect), the thrombus can pass through to the left side of the heart and into the systemic circulation. If it travels to the brain, it can cause a large stroke.
Risk Factors
- Immobility
- Recent surgery
- Long haul travel
- Pregnancy
- Hormone therapy with oestrogen
- Malignancy
- Polycythaemia
- Systemic lupus erythematosus
- Thrombophilia
TOM TIP: In your exams, when a patient presents with possible features of a DVT or PE, ask about risk factors such as periods of immobility, surgery and long-haul flights to score extra points.
Thrombophilias
Thrombophilias are conditions that predispose patients to develop blood clots. There are a large number of these:
- Antiphospholipid syndrome
- Factor V Leiden
- Antithrombin deficiency
- Protein C or S deficiency
- Hyperhomocysteinaemia
- Prothombin gene variant
- Activated protein C resistance
TOM TIP: The cause of recurrent venous thromboembolism to remember is antiphospholipid syndrome, which is associated with recurrent miscarriage and diagnosed with a blood test for antiphospholipid antibodies.
VTE Prophylaxis
Every patient admitted to hospital is assessed for their risk of venous thromboembolism (VTE). Patients at increased risk receive prophylaxis unless contraindicated. Prophylaxis usually involves low molecular weight heparin (LMWH), such as enoxaparin. Contraindications include active bleeding or existing anticoagulation with warfarin or a DOAC.
Anti-embolic compression stockings are also used. Peripheral arterial disease is the main contraindication for compression stockings.
DVT Presentation
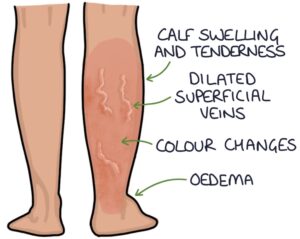
DVTs are almost always unilateral. Bilateral DVT is rare and bilateral symptoms are more likely due to an alternative diagnosis, such as chronic venous insufficiency or heart failure. DVTs can present with:
- Calf or leg swelling
- Dilated superficial veins
- Tenderness to the calf (particularly over the site of the deep veins)
- Oedema
- Colour changes to the leg
The calf circumference is measured 10cm below the tibial tuberosity. More than a 3cm difference is significant.
Consider a pulmonary embolism (e.g., shortness of breath and chest pain) in patients with features of a DVT.
Wells Score
The Wells score predicts the risk of a patient presenting with symptoms having a DVT or PE. It includes risk factors (e.g., recent surgery) and clinical findings (e.g., unilateral calf swelling over 3cm greater than the other leg).
Diagnosis
The Wells score is used when considering deep vein thrombosis. The outcome decides the next step:
- Likely: perform a leg vein ultrasound
- Unlikely: perform a d-dimer, and if positive, perform a leg vein ultrasound
D-dimer is a sensitive (95%) but not a specific blood test for VTE. It helps exclude VTE where there is a low suspicion. It is almost always raised if there is a DVT or PE. However, other conditions can cause a raised d-dimer:
- Pneumonia
- Malignancy
- Heart failure
- Surgery
- Pregnancy
Ultrasound of the leg is required to diagnose deep vein thrombosis. NICE recommends repeating negative ultrasound scans after 6-8 days if the patient has a positive D-dimer and the Wells score suggests a DVT is likely.
CT pulmonary angiogram (CTPA) is the usual first-line imaging investigation for a pulmonary embolism.
Initial Management
In most patients, NICE (2020) recommend treatment-dose apixaban or rivaroxaban as the initial anticoagulant. Low molecular weight heparin (LMWH) is the main alternative. This should be started immediately in patients where a DVT or PE is suspected and there is a delay in getting a scan to confirm the diagnosis.
The NICE guidelines (2020) recommend considering catheter-directed thrombolysis in patients with a symptomatic iliofemoral DVT and symptoms lasting less than 14 days. A catheter is inserted under x-ray guidance through the venous system to apply thrombolysis directly into the clot.
Long-Term Anticoagulation
The options for long-term anticoagulation in VTE are a DOAC, warfarin or LMWH.
Direct-acting oral anticoagulants (DOACs) are oral anticoagulants that do not require monitoring. Options are apixaban, rivaroxaban, edoxaban and dabigatran. They are suitable for most patients. Exceptions include severe renal impairment (creatinine clearance less than 15 ml/min), antiphospholipid syndrome and pregnancy.
Warfarin is a vitamin K antagonist. The target INR for warfarin is between 2 and 3 when treating DVTs and PEs. It is the first line in patients with antiphospholipid syndrome (who require initial concurrent treatment with LMWH).
Low molecular weight heparin (LMWH) is the first-line anticoagulant in pregnancy.
Anticoagulation is continued for:
- 3 months with a reversible cause (then review)
- 3-6 months in active cancer (then review)
- Long-term for unprovoked VTE, recurrent VTE or an irreversible underlying cause (e.g., thrombophilia)
Inferior Vena Cava Filter
Inferior vena cava filters are devices inserted into the inferior vena cava, designed to filter the blood and catch any blood clots travelling from the venous system towards the heart and lungs. They act as a sieve, allowing blood to flow through whilst stopping larger blood clots. They are used in those unsuitable for anticoagulation or where a PE has occurred whilst already on anticoagulation.
Investigating Unprovoked DVT
When patients have their first VTE without a clear cause, NICE (2020) recommend reviewing the medical history, baseline blood results and physical examination for evidence of cancer.
In patients with an unprovoked DVT or PE that are not going to continue anticoagulation beyond 3-6 months, NICE recommend considering testing for:
- Antiphospholipid syndrome (check antiphospholipid antibodies)
- Hereditary thrombophilias (only if they have a first-degree relative also affected by a DVT or PE)
Budd-Chiari Syndrome
Budd-Chiari syndrome involves obstruction to the outflow of blood from the liver caused by thrombosis in the hepatic veins or inferior vena cava. It is associated with hypercoagulable states (e.g., myeloproliferative disorders). It presents with a classic triad of:
- Abdominal pain
- Hepatomegaly
- Ascites
Doppler ultrasonography is the usual imaging investigation for establishing the diagnosis.
Treatment options include:
- Anticoagulation (e.g., low molecular weight heparin and warfarin)
- Endovascular procedures (e.g., thrombolysis or angioplasty)
- Transjugular intrahepatic portosystemic shunt (TIPS)
- Liver transplant
Last updated August 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

