Myeloproliferative disorders involve the uncontrolled proliferation of a single type of stem cell. They are considered a form of cancer occurring in the bone marrow, although they tend to develop and progress slowly. They have the potential to transform into acute myeloid leukaemia.
The myeloproliferative disorders to remember are:
- Primary myelofibrosis
- Polycythaemia vera
- Essential thrombocythaemia
|
Disease |
Proliferating Cell Line |
Blood Finding |
|
Primary Myelofibrosis |
Haematopoietic stem cells |
Low haemoglobin High or low white cell count High or low platelet count |
|
Polycythaemia Vera |
Erythroid cells |
High haemoglobin |
|
Essential Thrombocythaemia |
Megakaryocyte |
High platelet count |
These conditions are associated with mutations in certain genes:
- JAK2
- MPL
- CALR
TOM TIP: The mutation to remember is JAK2. Treatment might involve JAK2 inhibitors, such as ruxolitinib.
Myelofibrosis
Myelofibrosis can result from primary myelofibrosis, polycythaemia vera or essential thrombocythaemia.
Myelofibrosis is where the proliferation of a single cell line leads to bone marrow fibrosis, where bone marrow is replaced by scar tissue. This is in response to cytokines released from the proliferating cells. One particular cytokine is fibroblast growth factor. Fibrosis affects the production of blood cells and can lead to low haemoglobin (anaemia), low white blood cells (leukopenia) and low platelets (thrombocytopenia).
When the bone marrow is replaced with scar tissue, the production of blood cells (haematopoiesis) starts to happen in other areas, known as extramedullary haematopoiesis. Production of blood cells in the liver and spleen causes hepatomegaly, splenomegaly, and portal hypertension. When it occurs around the spine, it can cause spinal cord compression.
A blood film in myelofibrosis can show:
- Teardrop-shaped red blood cells
- Anisocytosis (varying sizes of red blood cells)
- Blasts (immature red and white cells)
Presentation
Initially, myeloproliferative disorders may be asymptomatic.
They can present with non-specific symptoms:
- Fatigue
- Weight loss
- Night sweats
- Fever
There may be signs and symptoms of underlying complications:
- Anaemia (tiredness, shortness of breath and dizziness)
- Splenomegaly (abdominal pain)
- Portal hypertension (ascites, varices and abdominal pain)
- Low platelets (bleeding and petechiae)
- Raised haemoglobin (itching, headaches and a red face)
- Low white blood cells (infections)
- Gout is a complication of polycythaemia
Thrombosis is a common complication of polycythaemia and thrombocythaemia, leading to myocardial infarction, stroke or venous thromboembolism (e.g., DVT and PE).
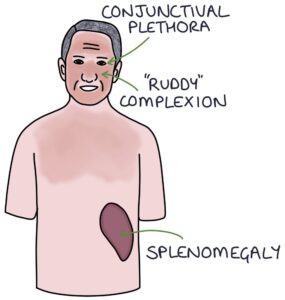
Clinical signs of polycythaemia include:
- Ruddy complexion (red face)
- Conjunctival plethora (the opposite of conjunctival pallor)
- Splenomegaly
- Hypertension
Diagnosis
Bone marrow biopsy is required to confirm the diagnosis. Bone marrow aspiration may be “dry” with myelofibrosis, as the bone marrow has turned to scar tissue.
Testing for the JAK2, MPL and CALR genes can help with diagnosis and management.
Management
Management of primary myelofibrosis may involve:
- No active treatment for mild disease with minimal symptoms
- Supportive management of complications, such as anaemia, splenomegaly and portal hypertension
- Chemotherapy (e.g., hydroxycarbamide) to help control the disease
- Targeted therapies, such as JAK2 inhibitors (ruxolitinib)
- Allogeneic stem cell transplantation (risky but potentially curative)
Management of polycythaemia vera may involve:
- Venesection to keep the haemoglobin in the normal range
- Aspirin to reduce the risk of thrombus formation
- Chemotherapy (typically hydroxycarbamide) to help control the disease
Management of essential thrombocythaemia may involve:
- Aspirin to reduce the risk of thrombus formation
- Chemotherapy (typically hydroxycarbamide) to help control the disease
- Anagrelide is a specialist platelet-lowering agent
Last updated August 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

