Brain tumours range from benign (e.g., meningiomas) to highly malignant (e.g., glioblastomas).
Presentation
Brain tumours may be asymptomatic, particularly when they are small. As they grow, they present with progressive focal neurological symptoms depending on the location of the lesion.
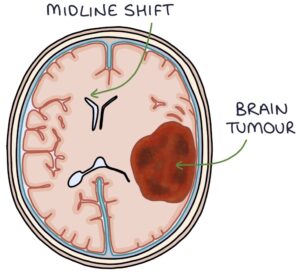
Brain tumours often present with symptoms and signs of raised intracranial pressure (intracranial hypertension). A growing tumour takes up room within the skull, leaving less space for the other contents (such as the cerebrospinal fluid), causing a rise in the pressure within the intracranial space.
TOM TIP: A common exam scenario is an unusual change in personality and behaviour, which indicates a frontal lobe tumour. The frontal lobe is responsible for personality and higher-level decision-making.
Intracranial Hypertension
The causes of increased pressure in the intracranial space include:
- Brain tumours
- Intracranial haemorrhage
- Idiopathic intracranial hypertension
- Abscesses or infection
In patients presenting with headaches, the concerning features that may indicate intracranial hypertension include:
- Constant headache
- Nocturnal (occurring at night)
- Worse on waking
- Worse on coughing, straining or bending forward
- Vomiting
- Papilloedema on fundoscopy
Other presenting features of raised intracranial hypertension may include:
- Altered mental state
- Visual field defects
- Seizures (particularly partial seizures)
- Unilateral ptosis (drooping upper eyelid)
- Third and sixth nerve palsies
Papilloedema
Papilloedema is a crucial fundoscopy finding in patients with increased intracranial pressure. Papilloedema describes swelling of the optic disc secondary to raised intracranial pressure. Papill- refers to a small, rounded, raised area (the optic disc) and -oedema refers to the swelling.
The sheath around the optic nerve is connected with the subarachnoid space. The raised cerebrospinal fluid (CSF) pressure flows into the optic nerve sheath, increasing the pressure around the optic nerve behind the optic disc causing the optic disc to bulge forward.
Papilloedema can be seen on fundoscopy as:
- Blurring of the optic disc margin
- Elevated optic disc (look for the way the retinal vessels flow across the disc to see the elevation)
- Loss of venous pulsation
- Engorged retinal veins
- Haemorrhages around the optic disc
- Paton’s lines, which are creases or folds in the retina around the optic disc
TOM TIP: When looking for the optic disc’s elevation, look at how the retinal vessels cross disc. Vessels can travel straight across a flat surface, whereas they will curve over a raised disc.
Gliomas
Gliomas are tumours of the glial cells in the brain or spinal cord. Glial cells surround and support the neurones. Glial cells include astrocytes, oligodendrocytes and ependymal cells.
Gliomas are graded from 1 to 4. Grade 1 is the most benign (possibly curable with surgery), and grade 4 is the most malignant (e.g., glioblastoma multiforme). The main three types (roughly from most to least malignant) are:
- Astrocytoma (the most common and aggressive form is glioblastoma)
- Oligodendroglioma
- Ependymoma
Meningiomas
Meningiomas are tumours growing from the cells of the meninges. They are usually benign. However, they take up space, and this “mass effect” can lead to raised intracranial pressure and neurological symptoms.
Secondary Metastases
The cancers that most often spread to the brain are:
- Lung
- Breast
- Renal cell carcinoma
- Melanoma
Pituitary Tumours
Pituitary tumours tend to be benign. If they grow large enough, they can press on the optic chiasm, causing a visual field defect called bitemporal hemianopia, with loss of the outer half of the visual fields in both eyes.
They can cause hormone deficiencies (hypopituitarism) or to release excessive hormones, leading to:
- Acromegaly (excessive growth hormone)
- Hyperprolactinaemia (excessive prolactin)
- Cushing’s disease (excessive ACTH and cortisol)
- Thyrotoxicosis (excessive TSH and thyroid hormone)
Pituitary tumours may be managed with:
- Trans-sphenoidal surgery (through the nose and sphenoid bone)
- Radiotherapy
- Bromocriptine to block excess prolactin
- Somatostatin analogues (e.g., octreotide) to block excess growth hormone
Acoustic Neuroma
Acoustic neuromas are benign tumours of the Schwann cells that surround the auditory nerve (vestibulocochlear nerve) that innervates the inner ear. Schwann cells provide the myelin sheath around neurones of the peripheral nervous system. Acoustic neuromas are also called vestibular schwannomas.
They occur at the cerebellopontine angle and are sometimes called cerebellopontine angle tumours.
They are usually unilateral. Bilateral acoustic neuromas are associated with neurofibromatosis type 2.
The typical patient is a 40-60 year old presenting with a gradual onset of:
- Unilateral sensorineural hearing loss (often the first symptom)
- Unilateral tinnitus
- Dizziness or imbalance
- Sensation of fullness in the ear
- Facial nerve palsy (if the tumour grows large enough to compress the facial nerve)
Management options include:
- Conservative management with monitoring may be used if there are no symptoms or treatment is inappropriate
- Surgery to remove the tumour (partial or total removal)
- Radiotherapy to reduce the growth
Management
MRI scan is the first-line investigation in patients with a possible brain tumour.
Biopsy gives the definitive histological diagnosis, usually obtained during surgery to remove the tumour.
The management of brain tumours depends on the type and grade, guided by the multidisciplinary team. The main options are:
- Surgery
- Chemotherapy
- Radiotherapy
- Palliative care
Last updated October 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

