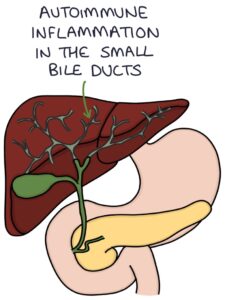
Primary biliary cholangitis is an autoimmune condition where the immune system attacks the small bile ducts in the liver, resulting in obstructive jaundice and liver disease. It was previously known as primary biliary cirrhosis.
Pathophysiology
Primary biliary cholangitis affects the small bile ducts inside the liver (the intrahepatic ducts). There is inflammation and damage to the epithelial cells of the bile ducts (the cholangiocytes). Over time, this can lead to obstruction of bile flow through these ducts. Reduced flow of bile is called cholestasis. The back-pressure of bile and the overall disease process ultimately lead to liver fibrosis, cirrhosis and failure.
Bile acids, bilirubin and cholesterol are excreted through the bile ducts into the intestines. When obstruction to the outflow of these chemicals means they are not being excreted, they build up in the blood. Raised bile acids cause itching, and raised bilirubin causes jaundice.
Raised cholesterol causes cholesterol deposits in the skin called xanthelasma. Xanthomas are larger nodular deposits of cholesterol in the skin or tendons. Raised cholesterol increases the risk of atherosclerosis and cardiovascular disease.
Bile acids help with the digestion of fats. Reduced or absent bile acids in the gastrointestinal tract cause abdominal symptoms, malabsorption of fat and greasy stools.
Bilirubin is responsible for the darker colour of stools. A lack of bilirubin results in pale stools. Excretion of bilirubin via the urine causes dark urine.
Presentation
The typical patient is a white woman aged 40-60 years. Often patients are asymptomatic at diagnosis, with the problem picked up on abnormal liver function tests. However, they may present with:
- Fatigue
- Pruritus (itching)
- Gastrointestinal symptoms and abdominal pain
- Jaundice
- Pale, greasy stools
- Dark urine
On examination, there may be:
- Xanthoma and xanthelasma (cholesterol deposits)
- Excoriations (scratches on the skin due to itching)
- Hepatomegaly
- Signs of liver cirrhosis and portal hypertension in end-stage disease (e.g., splenomegaly and ascites)
Investigations
Liver function tests show:
- Raise alkaline phosphatase (the most notable liver enzyme as with most “obstructive” pathology)
- Other liver enzymes and bilirubin are raised later in the disease
Autoantibodies relevant to primary biliary cholangitis are:
- Anti-mitochondrial antibodies (AMA) are the most specific to PBC and form part of the diagnostic criteria
- Anti-nuclear antibodies are present in about 35% of patients
Raised immunoglobulin M (IgM) is a non-specific blood result finding.
Ultrasound does not show specific changes with primary biliary cholangitis but helps exclude other pathology.
Liver biopsy may be used in diagnosing and staging the disease.
TOM TIP: The two results for primary biliary cholangitis to remember are anti-mitochondrial antibodies and alkaline phosphatase. In your exams, a middle-aged white woman presenting with itching, a positive AMA and a raised alkaline phosphatase almost certainly has primary biliary cholangitis.
Treatment
Ursodeoxycholic acid is the most essential treatment to remember in primary biliary cholangitis. It is a non-toxic, hydrophilic bile acid that protects the cholangiocytes from inflammation and damage. It makes the bile less harmful to the epithelial cells of the bile ducts. It slows the disease progression and improves outcomes.
Other treatments include:
- Obeticholic acid (where UDCA is inadequate or not tolerated – although it can have significant adverse effects)
- Colestyramine for symptoms of pruritus (a bile acid sequestrant that reduces intestinal absorption of bile acids)
- Replacement of fat-soluble vitamins
- Immunosuppression (e.g., with steroids) is considered in some patients
- Liver transplant in end-stage liver disease
Disease Progression
Disease course and symptoms vary significantly. Some people live decades without symptoms. The most crucial result is liver cirrhosis with the associated complications (e.g., portal hypertension and hepatocellular carcinoma).
Other complications and associations include:
- Fat-soluble vitamin deficiency (A, D, E and K)
- Osteoporosis
- Hyperlipidaemia (raised cholesterol)
- Sjögren’s syndrome (dry eyes, dry mouth and vaginal dryness)
- Connective tissue diseases (e.g., systemic sclerosis)
- Thyroid disease
Last updated May 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

