Arrhythmias are abnormal heart rhythms. They result from an interruption to the normal electrical signals that coordinate the contraction of the heart muscle. There are several types of arrhythmia, each with different causes and management options.
This section is a summary to help with exam preparation and is based on the guidelines from the Resuscitation Council UK from 2021. Attend the relevant courses, follow full guidelines and involve experienced seniors when treating patients.
Cardiac Arrest Rhythms
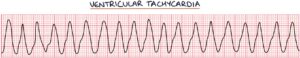
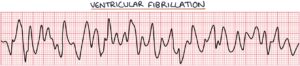
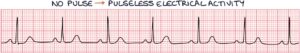
These are the four possible rhythms in a pulseless patient. They are either shockable (meaning defibrillation may be effective) or non-shockable (meaning defibrillation will not be effective).
Shockable rhythms:
- Ventricular tachycardia
- Ventricular fibrillation
Non-shockable rhythms:
- Pulseless electrical activity (all electrical activity except VF/VT, including sinus rhythm without a pulse)
- Asystole (no significant electrical activity)

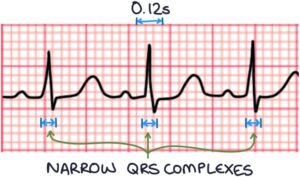
Narrow Complex Tachycardia
Narrow complex tachycardia refers to a fast heart rate with a QRS complex duration of less than 0.12 seconds. On a normal 25 mm/sec ECG, 0.12 seconds equals 3 small squares. Therefore, the QRS complex will fit within 3 small squares in narrow complex tachycardia.
There are four main differentials of a narrow complex tachycardia:
- Sinus tachycardia (treatment focuses on the underlying cause)
- Supraventricular tachycardia (treated with vagal manoeuvres and adenosine)
- Atrial fibrillation (treated with rate control or rhythm control)
- Atrial flutter (treated with rate control or rhythm control, similar to atrial fibrillation)
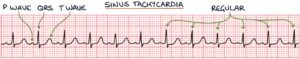
Sinus tachycardia will take the normal P wave, QRS complex and T wave pattern. Sinus tachycardia is not an arrhythmia and is usually a response to an underlying cause, such as sepsis or pain.
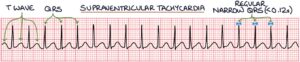
Supraventricular tachycardia (SVT) looks like a QRS complex followed immediately by a T wave, then a QRS complex, then a T wave, and so on. There are P waves, but they are often buried in the T waves, so you cannot see them. It can be distinguished from atrial fibrillation by the regular rhythm and atrial flutter by the absence of a saw-tooth pattern.
It can be tricky to distinguish SVT from sinus tachycardia. SVT has an abrupt onset and a very regular pattern without variability. Sinus tachycardia has a more gradual onset and more variability in the rate. The history is also important, where sinus tachycardia usually has an explanation (e.g., pain or fever), while SVT can appear at rest with no apparent cause.
Atrial fibrillation can be identified on an ECG by absent P waves and an irregularly irregular ventricular rhythm.

In atrial flutter, the atrial rate is usually around 300 beats per minute and gives a saw-tooth pattern on the ECG. A QRS complex occurs at regular intervals depending on how often there is conduction from the atria. This often results in two atrial contractions for every one ventricular contraction, giving a ventricular rate of 150 beats per minute.

Patients with life-threatening features, such as loss of consciousness (syncope), heart muscle ischaemia (e.g., chest pain), shock or severe heart failure, are treated with synchronised DC cardioversion under sedation or general anaesthesia. Intravenous amiodarone is added if initial DC shocks are unsuccessful.
Broad Complex Tachycardia
Broad complex tachycardia refers to a fast heart rate with a QRS complex duration of more than 0.12 seconds or 3 small squares on an ECG.
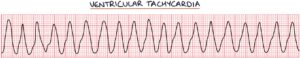
The resuscitation guidelines break down broad complex tachycardia into:
- Ventricular tachycardia or unclear cause (treated with IV amiodarone)
- Polymorphic ventricular tachycardia, such as torsades de pointes (treated with IV magnesium)
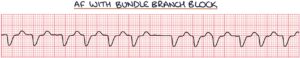
- Atrial fibrillation with bundle branch block (treated as AF)
- Supraventricular tachycardia with bundle branch block (treated as SVT)


Patients with life-threatening features, such as loss of consciousness (syncope), heart muscle ischaemia (e.g., chest pain), shock or severe heart failure, are treated with synchronised DC cardioversion under sedation or general anaesthesia. Intravenous amiodarone is added if initial DC shocks are unsuccessful.
Atrial Flutter
Normally the electrical signal passes through the atria once, stimulating a contraction, then disappears through the atrioventricular node into the ventricles. Atrial flutter is caused by a re-entrant rhythm in either atrium. The electrical signal re-circulates in a self-perpetuating loop due to an extra electrical pathway in the atria. The signal goes round and round the atrium without interruption. The atrial rate is usually around 300 beats per minute.

Atrial flutter gives a sawtooth appearance on the ECG, with repeated P wave occurring at around 300 per minute, with a narrow complex tachycardia.
The signal does not usually enter the ventricles on every lap due to the long refractory period of the atrioventricular node. This often results in two atrial contractions for every one ventricular contraction (2:1 conduction), giving a ventricular rate of 150 beats per minute.

There may be 3:1, 4:1 or variable conduction ratios.

Treatment is similar to atrial fibrillation, including anticoagulation based on the CHA2DS2-VASc score. Radiofrequency ablation of the re-entrant rhythm can be a permanent solution.
Prolonged QT Interval
The QT interval is from the start of the QRS complex to the end of the T wave. The corrected QT interval (QTc) estimates the QT interval if the heart rate were 60 beats per minute. It is prolonged at:
- More than 440 milliseconds in men
- More than 460 milliseconds in women
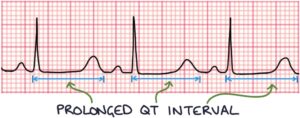
A prolonged QT interval represents prolonged repolarisation of the heart muscle cells (myocytes) after a contraction. Depolarisation is the electrical process that leads to heart contraction. Repolarisation is a recovery period before the muscle cells are ready to depolarise again. Waiting a long time for repolarisation can result in spontaneous depolarisation in some muscle cells. These abnormal spontaneous depolarisations before repolarisation are known as afterdepolarisations. These afterdepolarisations spread throughout the ventricles, causing a contraction before proper repolarisation. When this leads to recurrent contractions without normal repolarisation, it is called torsades de pointes.
Torsades de pointes is a type of polymorphic ventricular tachycardia. It translates from French as “twisting of the spikes”, describing the ECG characteristics. On an ECG, it looks like standard ventricular tachycardia but with the appearance that the QRS complex is twisting around the baseline. The height of the QRS complexes gets progressively smaller, then larger, then smaller, and so on.

Torsades de pointes will terminate spontaneously and revert to sinus rhythm or progress to ventricular tachycardia. Ventricular tachycardia can lead to cardiac arrest.
Causes of prolonged QT include:
- Long QT syndrome (an inherited condition)
- Medications, such as antipsychotics, citalopram, flecainide, sotalol, amiodarone and macrolide antibiotics
- Electrolyte imbalances, such as hypokalaemia, hypomagnesaemia and hypocalcaemia
Management of a prolonged QT interval involves:
- Stopping and avoiding medications that prolong the QT interval
- Correcting electrolyte disturbances
- Beta blockers (not sotalol)
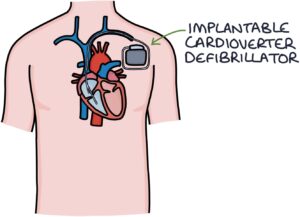
- Pacemakers or implantable cardioverter defibrillators
Acute management of torsades de pointes involves:
- Correcting the underlying cause (e.g., electrolyte disturbances or medications)
- Magnesium infusion (even if they have normal serum magnesium)
- Defibrillation if ventricular tachycardia occurs
Ventricular Ectopics
Ventricular ectopics are premature ventricular beats caused by random electrical discharges outside the atria. Patients often present complaining of random extra or missed beats. They are relatively common at all ages and in healthy patients. However, they are more common in patients with pre-existing heart conditions (e.g., ischaemic heart disease or heart failure).
Ventricular ectopics appear as isolated, random, abnormal, broad QRS complexes on an otherwise normal ECG.
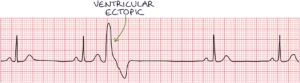
Bigeminy refers to when every other beat is a ventricular ectopic. The ECG shows a normal beat (with a P wave, QRS complex and T wave), followed immediately by an ectopic beat, then a normal beat, then an ectopic, and so on.

Management involves:
- Reassurance and no treatment in otherwise healthy people with infrequent ectopics
- Seeking specialist advice in patients with underlying heart disease, frequent or concerning symptoms (e.g., chest pain or syncope), or a family history of heart disease or sudden death
- Beta blockers are sometimes used to manage symptoms
Heart Block
First-degree heart block occurs where there is delayed conduction through the atrioventricular node. Despite this, every atrial impulse leads to a ventricular contraction, meaning every P wave is followed by a QRS complex. On an ECG, first-degree heart block presents as a PR interval greater than 0.2 seconds (5 small or 1 big square).

Second-degree heart block is where some atrial impulses do not make it through the atrioventricular node to the ventricles. There are instances where P waves are not followed by QRS complexes. There are two types of second-degree heart block:
- Mobitz type 1 (Wenckebach phenomenon)
- Mobitz type 2
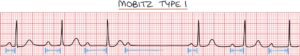
Mobitz type 1 (Wenckebach phenomenon) is where the conduction through the atrioventricular node takes progressively longer until it finally fails, after which it resets, and the cycle restarts. On an ECG, there is an increasing PR interval until a P wave is not followed by a QRS complex. The PR interval then returns to normal, and the cycle repeats itself.
Mobitz type 2 is where there is intermittent failure of conduction through the atrioventricular node, with an absence of QRS complexes following P waves. The PR interval remains normal. There is a risk of asystole with Mobitz type 2.
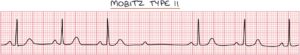
There is usually a set ratio of P waves to QRS complexes, for example, three P waves for each QRS complex (3:1 block).
A 2:1 block is where there are two P waves for each QRS complex. Every other P wave does not stimulate a QRS complex. It can be difficult to tell whether this is caused by Mobitz type 1 or Mobitz type 2.

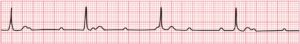
Third-degree heart block is also called complete heart block. There is no observable relationship between the P waves and QRS complexes. There is a significant risk of asystole with third-degree heart block.
Bradycardias
Bradycardia refers to a slow heart rate, typically less than 60 beats per minute. A heart rate under 60 can be normal in healthy fit patients without causing any symptoms. There is a long list of causes of bradycardia, including:
- Medications (e.g., beta blockers)
- Heart block
- Sick sinus syndrome
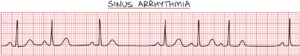
Sick sinus syndrome encompasses many conditions that cause dysfunction in the sinoatrial node. It is often caused by idiopathic degenerative fibrosis of the sinoatrial node. It can result in sinus bradycardia, sinus arrhythmias and prolonged pauses.
Asystole refers to the absence of electrical activity in the heart (resulting in cardiac arrest). There is a risk of asystole in:
- Mobitz type 2
- Third-degree heart block (complete heart block)
- Previous asystole
- Ventricular pauses longer than 3 seconds
Management of unstable patients and those at risk of asystole involves:
- Intravenous atropine (first line)
- Inotropes (e.g., isoprenaline or adrenaline)
- Temporary cardiac pacing
- Permanent implantable pacemaker, when available
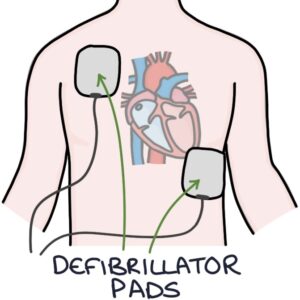
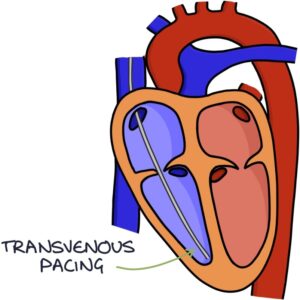
Options for temporary cardiac pacing are:
- Transcutaneous pacing, using pads on the patient’s chest
- Transvenous pacing, using a catheter, fed through the venous system to stimulate the heart directly
Atropine is an antimuscarinic medication and works by inhibiting the parasympathetic nervous system. Inhibiting the parasympathetic nervous system leads to side effects of pupil dilation, dry mouth, urinary retention and constipation.
Last updated April 2024
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.


