Tetralogy of Fallot is a congenital condition involving four coexisting pathologies:
- Ventricular septal defect (VSD)
- Overriding aorta
- Pulmonary valve stenosis
- Right ventricular hypertrophy
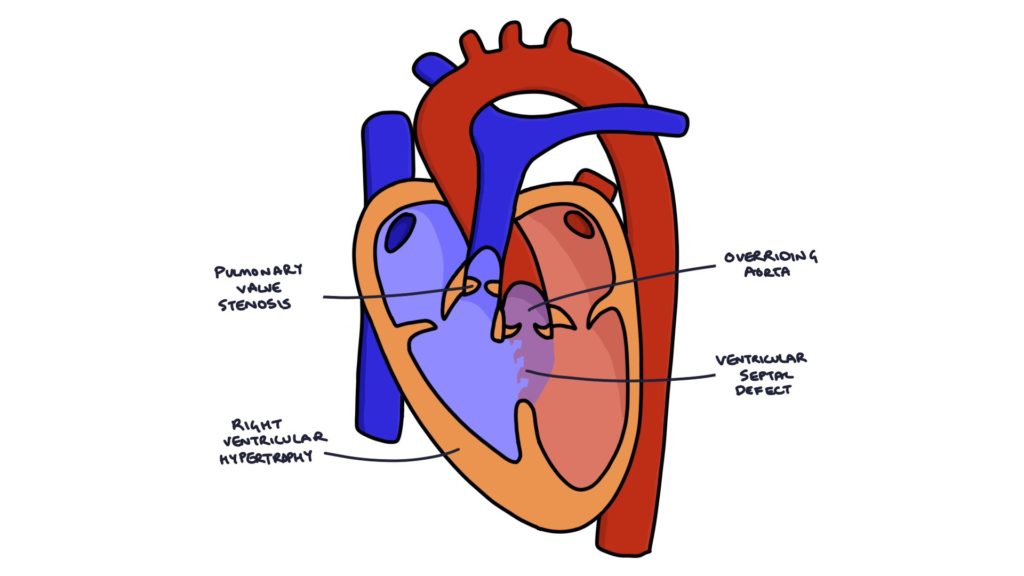
Overriding aorta refers to when the entrance to the aorta is placed further to the right than normal, above the ventricular septal defect. When the right ventricle contracts, squeezing blood upwards, the aorta is in the direction of travel of that blood, causing deoxygenated blood to enter the aorta, bypassing the lungs.
Pulmonary valve stenosis encourages blood to flow through the VSD and into the aorta rather than through the pulmonary valve into the pulmonary vessels.
The increased strain on the right ventricle as it pumps blood against the resistance of the left ventricle and pulmonary stenosis causes right ventricular hypertrophy, with thickening of the heart muscle.
The overriding aorta and pulmonary stenosis encourage blood to be shunted from the right heart to the left, bypassing the lung. This right-to-left cardiac shunt means deoxygenated blood bypasses the child’s lungs and enters the systemic circulation, causing cyanosis. The severity of pulmonary stenosis determines the degree of cyanosis.
Risk Factors
Risk factors and associations include:
- Increased maternal age (over 40 years)
- Alcohol consumption in pregnancy
- Maternal diabetes
- Genetic conditions (e.g., DiGeorge syndrome and Down’s syndrome)
- Congenital rubella syndrome
Presentation
Most cases are identified during the antenatal scans.
Signs and symptoms include:
- Shortness of breath
- Cyanosis
- Finger clubbing
- Poor feeding
- Poor weight gain
- Tet spells (intermittent episodes of cyanosis)
Tetralogy of Fallot produces an ejection systolic murmur heard loudest in the pulmonary area (second intercostal space, left sternal border).
Investigations
An echocardiogram confirms the diagnosis. Doppler can show the direction of blood flow.
A chest x-ray may show the characteristic “boot-shaped” heart due to right ventricular thickening.
Management
In neonates, a prostaglandin E1 infusion may be used to maintain the ductus arteriosus. This allows blood to flow from the aorta to the pulmonary arteries. A stent may be inserted to keep the ductus arteriosus open.
A Blalock-Taussig shunt involves creating a connection between a systemic artery (e.g., the left subclavian artery) and a pulmonary artery, increasing blood flow to the lungs. This may be used as a temporary measure in neonates who are too small for total repair.
Total surgical repair by open heart surgery is the definitive treatment.
Tet Spells
Tet spells are intermittent cyanotic episodes caused by a temporary worsening of the right-to-left shunt. They occur when the pulmonary vascular resistance increases or the systemic resistance decreases. For example, extra carbon dioxide is generated during physical exertion, which is a vasodilator that reduces systemic vascular resistance. Reduced systemic vascular resistance encourages blood to flow from the right ventricle to the aorta rather than to the pulmonary vessels and lungs.
These episodes may be precipitated by waking, physical exertion or crying. The child becomes irritable, cyanotic and short of breath. Severe spells can lead to reduced consciousness, seizures and potentially death.
Management of Tet Spells
Older children may squat when a tet spell occurs. Younger children can be placed in the “knees to chest” position. Squatting increases systemic vascular resistance, encouraging blood to enter the pulmonary vessels.
Medical management (under senior supervision) may involve:
- Oxygen
- IV morphine (decreases respiratory drive and pulmonary vascular resistance)
- IV fluids (increases circulating volume)
- IV beta blockers (e.g., propranolol)
- Phenylephrine infusion (increases systemic vascular resistance)
Last updated January 2025
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

