Atherosclerosis
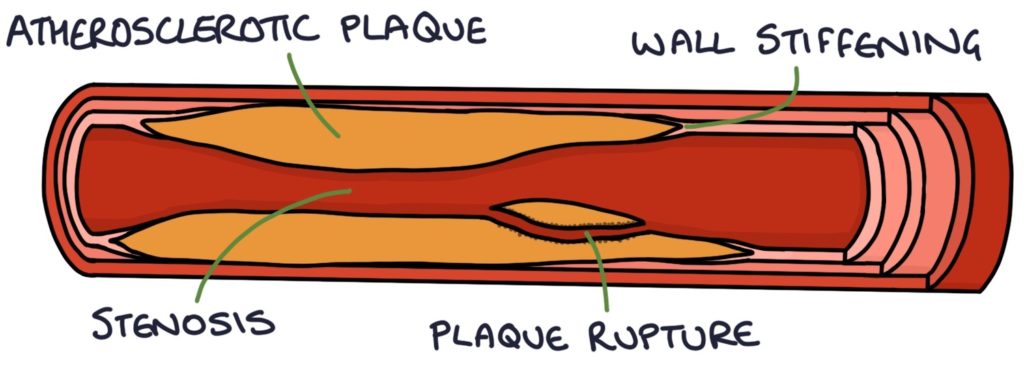
Athero- refers to soft or “porridge-like”, and -sclerosis refers to hardening. Atherosclerosis is a combination of atheromas (fatty deposits in the artery walls) and sclerosis (hardening or stiffening of the blood vessel walls).
Atherosclerosis affects the medium and large arteries. It is caused by chronic inflammation and activation of the immune system in the artery wall. This causes the deposition of lipids in the artery wall, followed by the development of fibrous atheromatous plaques.
These plaques result in:
- Stiffening
- Stenosis
- Plaque rupture
Stiffening of the artery walls leads to hypertension (raised blood pressure) and strain on the heart as it tries to pump blood against extra resistance.
Stenosis leads to reduced blood flow (e.g. in angina).
Plaque rupture creates a thrombus that can block a distal vessel and cause ischaemia. An example is acute coronary syndrome, where a coronary artery becomes blocked.
Risk Factors
It is important to separate the risk factors for cardiovascular disease into modifiable and non-modifiable risk factors. There is nothing we can do about non-modifiable risk factors, but we can do something about the modifiable ones.
Non-modifiable risk factors:
- Older age
- Family history
- Male
Modifiable risk factors:
- Raised cholesterol
- Smoking
- Alcohol consumption
- Poor diet
- Lack of exercise
- Obesity
- Poor sleep
- Stress
Medical Co-Morbidities
Medical co-morbidities increase the risk of atherosclerosis and should be carefully managed to minimise the risk:
- Diabetes
- Hypertension
- Chronic kidney disease (CKD)
- Inflammatory conditions, such as rheumatoid arthritis
- Atypical antipsychotic medications
TOM TIP: Consider risk factors when taking a history from someone with suspected atherosclerotic disease (such as someone presenting with chest pain). Ask about their exercise, diet, past medical history, family history, occupation, smoking, alcohol intake and medications. This will help you perform well in exams and when presenting to seniors.
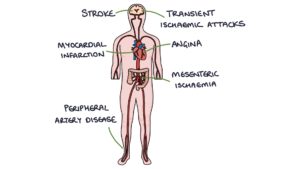
End Results of Atherosclerosis
- Angina
- Myocardial infarction
- Transient ischaemic attacks
- Strokes
- Peripheral arterial disease
- Chronic mesenteric ischaemia
Prevention of Cardiovascular Disease
Prevention of cardiovascular disease falls into two main categories:
- Primary prevention for patients that have never had a diagnosis of cardiovascular disease.
- Secondary prevention after a diagnosis of angina, myocardial infarction, TIA, stroke or peripheral arterial disease.
Optimise Modifiable Risk Factors
For primary and secondary prevention of cardiovascular disease, it is essential to optimise the modifiable risk factors:
- Address diet, exercise and obesity
- Stop smoking
- Reducing alcohol consumption
- Optimise treatment of co-morbidities (such as diabetes)
Diet and Exercise
The NICE guidelines on cardiovascular disease (updated February 2023) recommend the following dietary changes:
- Total fat is less than 30% of total calories (primarily monounsaturated and polyunsaturated fats)
- Saturated fat is less than 7% of total calories
- Reduced sugar intake
- Wholegrain options
- At least 5 a day of fruit and vegetables
- At least 2 a week of fish (one being oily)
- At least 4 a week of legumes, seeds and nuts
The NICE guidelines recommend (limited by co-morbidities):
- Aerobic activity for a total of at least 150 minutes at moderate intensity or 75 minutes at vigorous intensity per week
- Strength training activities at least 2 days a week
Primary Prevention of Cardiovascular Disease
Medication for primary prevention is based on the QRISK3 score.
The QRISK score estimates the percentage risk that a patient will have a stroke or myocardial infarction in the next 10 years. The NICE guidelines (updated February 2023) recommend when the result is above 10%, they should be offered a statin, initially atorvastatin 20mg at night.
Atorvastatin 20mg is offered as primary prevention to all patients with:
- Chronic kidney disease (eGFR less than 60 ml/min/1.73 m2)
- Type 1 diabetes for more than 10 years or are over 40 years
The draft NICE guidelines due for publication in mid-2023 advise that atorvastatin 20mg can be considered for primary prevention in patients with a QRISK3 score below 10%.
Statins
Statins reduce cholesterol production in the liver by inhibiting HMG CoA reductase.
NICE recommend checking lipids 3 months after starting statins and increasing the dose to aim for a greater than 40% reduction in non-HDL cholesterol. Check adherence (are they taking the medications?) before increasing the dose.
NICE also recommend checking LFTs within 3 months of starting a statin and again at 12 months. Statins can cause a transient and mild rise in ALT and AST in the first few weeks of use. They usually do not need to be stopped if the rise is less than 3 times the upper limit of normal.
Rare and significant side effects of statins include:
- Myopathy (causing muscle weakness and pain)
- Rhabdomyolysis (muscle damage – check the creatine kinase in patients with muscle pain)
- Type 2 diabetes
- Haemorrhagic strokes (very rarely)
Usually, the benefits of statins far outweigh the risks, and newer statins (such as atorvastatin) are well tolerated.
TOM TIP: Several common medications interact with statins. One key interaction to remember is with macrolide antibiotics. Patients being prescribed clarithromycin or erythromycin should be advised to stop taking their statin whilst taking these antibiotics.
Other Cholesterol Lowering Drugs
Ezetimibe works by inhibiting the absorption of cholesterol in the intestine. It can be used as an alternative when statins are not tolerated or in combination with a statin when statins alone are inadequate.
Ezetimibe may be combined with bempedoic acid, a drug that reduces cholesterol production in the liver.
PCSK9 inhibitors (e.g., evolocumab and alirocumab) are monoclonal antibodies that lower cholesterol. They are highly specialist treatments, given as a subcutaneous injection every 2-4 weeks.
Secondary Prevention of Cardiovascular Disease
Secondary prevention after developing cardiovascular disease depends on the specific condition. Secondary prevention can be remembered with the “4 As” mnemonic:
- A – Antiplatelet medications (e.g., aspirin, clopidogrel and ticagrelor)
- A – Atorvastatin 80mg
- A – Atenolol (or an alternative beta blocker – commonly bisoprolol) titrated to the maximum tolerated dose
- A – ACE inhibitor (commonly ramipril) titrated to the maximum tolerated dose
After a myocardial infarction, patients are offered dual antiplatelet treatment initially, with:
- Aspirin 75mg daily (continued indefinitely)
- Clopidogrel or ticagrelor (generally for 12 months before stopping)
Clopidogrel is the antiplatelet of choice in peripheral arterial disease and following an ischaemic stroke.
Familial Hypercholesterolaemia
Familial hypercholesterolaemia is an autosomal dominant genetic condition causing very high cholesterol levels. Several genes have the potential to cause the disorder.
Heterozygous means only one copy of the gene is abnormal. This occurs in about 1 in 250 people.
Homozygous means both copies of the gene are abnormal. This very rare condition causes extremely high cholesterol (over 13 mmol/L) and almost guaranteed early cardiovascular disease.
The Simon Broome criteria or the Dutch Lipid Clinic Network Criteria are used for making a clinical diagnosis. Three important features to remember are:
- Family history of premature cardiovascular disease (e.g., myocardial infarction under 60 in a first-degree relative)
- Very high cholesterol (e.g., above 7.5 mmol/L in an adult)
- Tendon xanthomata (hard nodules in the tendons containing cholesterol, often on the back of the hand and Achilles)
Management of familial hypercholesterolaemia involves:
- Specialist referral for genetic testing and testing of family members
- Statins
Last updated March 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

