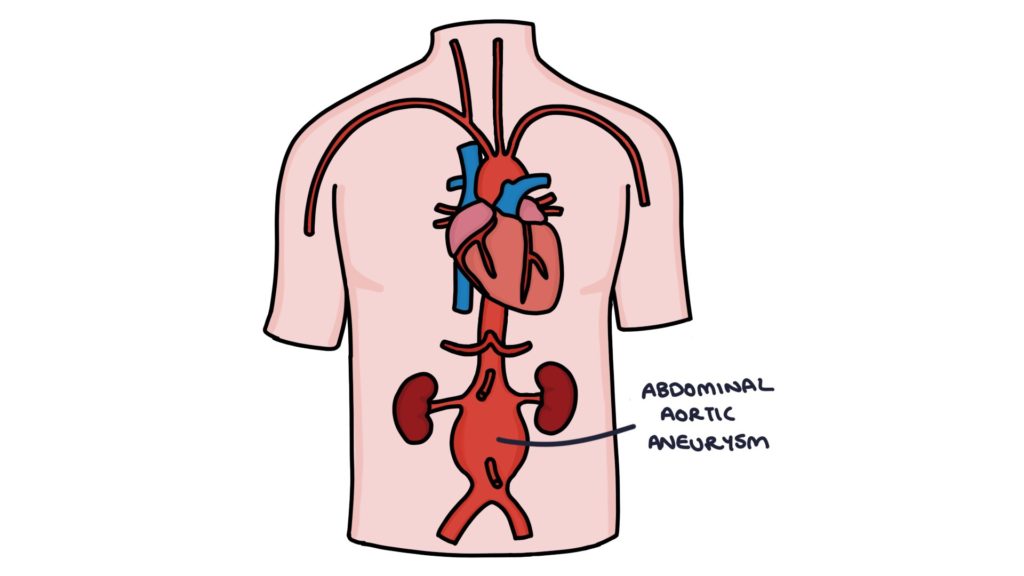
Abdominal aortic aneurysm (AAA) refers to dilation of the abdominal aorta, with a diameter of more than 3cm. Often the first time patients become aware of an aneurysm is when it ruptures, causing life-threatening bleeding into the abdominal cavity. The mortality of a ruptured AAA is around 80%.
Risk Factors
- Men are affected significantly more often and at a younger age than women
- Increased age
- Smoking
- Hypertension
- Family history
- Existing cardiovascular disease
Screening
All men in England are offered a screening ultrasound scan at age 65 to detect asymptomatic AAA. Early detection of an AAA means preventative measures can stop it from expanding further or rupturing.
Women are not routinely offered screening, as they are at much lower risk. The NICE guidelines (2020) say a routine ultrasound can be considered in women aged over 70 with risk factors such as existing cardiovascular disease, COPD, family history, hypertension, hyperlipidaemia or smoking.
Patients with an aorta diameter above 3cm are referred to a vascular team (urgently if more than 5.5cm).
Presentation
Most patients with an AAA are asymptomatic. It may be discovered on routine screening or when it ruptures.
Other ways it can present include:
- Non-specific abdominal pain
- Pulsatile and expansile mass in the abdomen when palpated with both hands
- As an incidental finding on an abdominal x-ray, ultrasound or CT scan
Diagnosis
Ultrasound is the usual initial investigation for establishing the diagnosis.
CT angiogram gives a more detailed picture of the aneurysm and helps guide elective surgery to repair the aneurysm.
Classification
The severity of the aortic aneurysm depends on the size:
- Normal: less than 3cm
- Small aneurysm: 3 – 4.4cm
- Medium aneurysm: 4.5 – 5.4cm
- Large aneurysm: above 5.5cm
Management
The risk of progression of an AAA can be reduced by treating reversible risk factors:
- Stop smoking
- Healthy diet and exercise
- Optimising the management of hypertension, diabetes and hyperlipidaemia
The Public Health England (updated 2017) screening and surveillance programme recommends follow up scans:
- Yearly for patients with aneurysms 3-4.4cm
- 3 monthly for patients with aneurysms 4.5-5.4cm
The NICE guidelines (2020) recommend elective repair for patients with any of:
- Symptomatic aneurysm
- Diameter growing more than 1cm per year
- Diameter above 5.5cm
Elective surgical repair involves inserting an artificial “graft” into the section of the aorta affected by the aneurysm. There are two methods for inserting the graft:
- Open repair via a laparotomy
- Endovascular aneurysm repair (EVAR) using a stent inserted via the femoral arteries
Gov.uk (April 2021) advise that patients must:
- Inform the DVLA if they have an aneurysm above 6cm
- Stop driving if it is above 6.5cm
- Stricter rules apply to drivers of heavy vehicles (e.g., bus or lorry drivers)
Ruptured AAA
The risk of rupture increases with the diameter of the aneurysm (roughly 5% for 5cm and 40% for 8 cm aneurysm). Ruptured AAA has an extremely high mortality (around 80%).
A ruptured aortic aneurysm presents with:
- Severe abdominal pain that may radiate to the back or groin
- Haemodynamic instability (hypotension and tachycardia)
- Pulsatile and expansile mass in the abdomen
- Collapse
- Loss of consciousness
An abdominal aortic aneurysm is a surgical emergency requiring immediate involvement of experienced seniors, vascular surgeons, anaesthetists and theatre teams.
Permissive hypotension refers to the strategy of aiming for a lower than normal blood pressure when performing fluid resuscitation. The theory is that increasing the blood pressure may increase blood loss.
Haemodynamically unstable patients with a suspected AAA should be transferred directly to theatre. Surgical repair should not be delayed by getting imaging to confirm the diagnosis.
CT angiogram can be used to diagnose or exclude ruptured AAA in haemodynamically stable patients.
In patients with co-morbidities that make the prognosis with surgery very poor, a discussion needs to be had with senior doctors, the patient and their family about palliative care.
Last updated May 2021
