Carpal tunnel syndrome is caused by compression of the medial nerve as it travels through the carpal tunnel in the wrist, causing pain and numbness in the median nerve distribution on the hand.
Basic Anatomy and Pathophysiology
The flexor retinaculum is a fibrous band that wraps across the front (palmar side) of the wrist. It is also known as the transverse carpal ligament. Between the carpal bones and the flexor retinaculum is a passageway from the forearm and the hand called the carpal tunnel. The median nerve and the flexor tendons of the forearm travel through the carpal tunnel.
Compression of the contents of the carpal tunnel (causing carpal tunnel syndrome) is the result of either:
- Swelling of the contents (e.g., swelling of the tendon sheaths due to repetitive strain)
- Narrowing of the tunnel
The palmar digital cutaneous branch of the median nerve (which passes through the carpal tunnel) is responsible for sensory innervation of the palmar aspects and full fingertips of the:
- Thumb
- Index and middle finger
- The lateral half of ring finger
Note that the palmar cutaneous branch of the median nerve provides sensation to the palm. However, this branch originates before the carpal tunnel and does not travel through the carpal tunnel. Therefore, it is not affected by carpal tunnel syndrome.
The median nerve also supplies the motor function to the three thenar muscles. These muscles make up the muscular bulge at the base of the thumb that is responsible for thumb movements:
- Abductor pollicis brevis (thumb abduction)
- Opponens pollicis (thumb opposition – reaching across the palm to touch the tips of the fingers)
- Flexor pollicis brevis (thumb flexion)
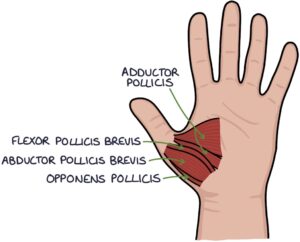
The other muscle that controls thumb movement is the adductor pollicis (thumb adduction). However, this is innervated by the ulnar nerve. Whether this is classed as one of the thenar muscles depends on where you look.
Risk Factors
In most cases, carpal tunnel syndrome is idiopathic, meaning no clear cause is found.
There are a number of key risk factors:
- Repetitive strain
- Obesity
- Perimenopause
- Rheumatoid arthritis
- Diabetes
- Acromegaly
- Hypothyroidism
TOM TIP: When I was preparing for the PACES exam, the link between bilateral carpal tunnel syndrome and acromegaly came up several times. Cases would present a patient with symptoms of bilateral carpal tunnel syndrome. The challenge was not only to diagnose carpal tunnel syndrome but also to identify the features of the underlying cause. Whenever you see a patient in an OSCE station that has a diagnosis, ask yourself whether that diagnosis might have an underlying cause and look for features of that cause. For example, if you see a patient with bilateral carpal tunnel syndrome, look for features that might suggest underlying rheumatoid arthritis, diabetes, acromegaly or hypothyroidism. This will take you from average exams scores to the very top scores.
Presentation
Carpal tunnel syndrome usually has a gradual onset of symptoms. Initially, the symptoms are intermittent. Often, they are worse at night time.
Carpal tunnel syndrome causes sensory symptoms in the distribution of the palmar digital cutaneous branch of the median nerve, affecting the palmar aspects and full fingertips of the:
- Thumb
- Index and middle finger
- The lateral half of ring finger
Sensory symptoms include:
- Numbness
- Paraesthesia (pins and needles or tingling)
- Burning sensation
- Pain
Patients often find the sensory symptoms worse at night. The symptoms may cause them to wake up from sleep. They may describe shaking their hand to try and relieve symptoms.
Motor symptoms of carpal tunnel syndrome affect the thenar muscles, with:
- Weakness of thumb movements
- Weakness of grip strength
- Difficulty with fine movements involving the thumb
- Wasting of the thenar muscles (muscle atrophy)
Special Tests
There are two special tests for carpal tunnel syndrome:
- Phalen’s test
- Tinel’s test
Phalen’s test involves fully flexing the wrist and holding it in this position. Often this is done by asking the patient to put the backs of their hands together in front of them with the wrists bent inwards at 90 degrees. The test is positive when this position triggers the sensory symptoms of carpal tunnel, with numbness and paraesthesia in the median nerve distribution.
Tinel’s test involves tapping the wrist at the location where the median nerve travels through the carpal tunnel. This is in the middle, at the point where the wrist meets the hand. The test is positive when this position triggers the sensory symptoms of carpal tunnel, with numbness and paraesthesia in the median nerve distribution.
TOM TIP: I think of tapping a tin can (Tinel’s) to remember the difference between Phalen’s and Tinel’s test.
Carpal Tunnel Questionnaire
The Kamath and Stothard carpal tunnel questionnaire (CTQ) gives a score based on the symptoms. It can be used to predict the likelihood of a diagnosis of carpal tunnel syndrome. A high score on the questionnaire may replace the need for nerve conduction studies to confirm the diagnosis.
It scores based on questions such as:
- Do symptoms wake you at night?
- Do you have trick movements (e.g., shaking the hand) to improve symptoms?
- Is your little finger affected? (Answering yes scores negatively, making carpal tunnel syndrome less likely)
Nerve Conduction Studies
Nerve conduction studies are the primary investigation for establishing the diagnosis.
A small electrical current is applied by an electrode (nerve stimulator) to the median nerve on one side of the carpal tunnel. Recording electrodes over the median nerve on the other side of the carpal tunnel record the electrical current that reaches them. This demonstrates how well signals are passing through the carpal tunnel along the median nerve.
Management
Management options for carpal tunnel syndrome are:
- Rest and altered activities
- Wrist splints that maintain a neutral position of the wrist can be worn at night (for a minimum of 4 weeks)
- Steroid injections
- Surgery
Carpal tunnel syndrome surgery is usually performed as a day case procedure under local anaesthetic. It can be performed by open (with a vertical incision at the wrist) or endoscopic (keyhole) surgery. The flexor retinaculum (AKA transverse carpal ligament) is cut to release the pressure on the median nerve.
Last updated August 2021
