Tetralogy of Fallot is a congenital condition where there are four coexisting pathologies:
- Ventricular septal defect (VSD)
- Overriding aorta
- Pulmonary valve stenosis
- Right ventricular hypertrophy
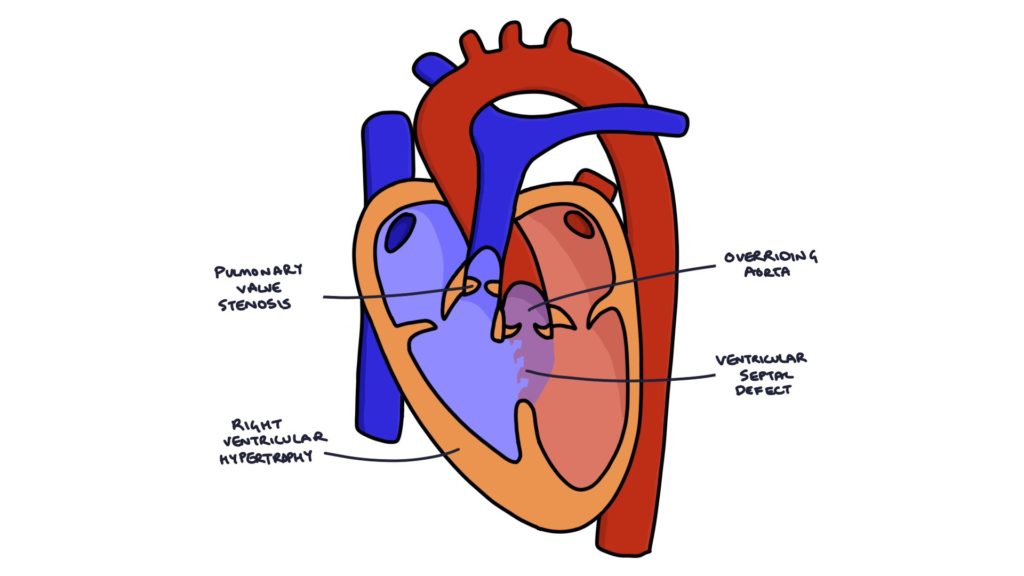
The VSD allows blood to flow between the ventricles. The term “overriding aorta” refers to the fact that the entrance to the aorta (the aortic valve) is placed further to the right than normal, above the VSD. This means that when the right ventricle contracts and sends blood upwards, the aorta is in the direction of travel of that blood, therefore a greater proportion of deoxygenated blood enters the aorta from the right side of the heart.
Stenosis of the pulmonary valve provides greater resistance against the flow of blood from the right ventricle. This encourages blood to flow through the VSD and into the aorta rather than taking the normal route into the pulmonary vessels. Therefore, the overriding aorta and pulmonary stenosis encourage blood to be shunted from the right heart to the left, causing cyanosis.
The increased strain on the muscular wall of the right ventricle as it attempts to pump blood against the resistance of the left ventricle and pulmonary stenosis causes right ventricular hypertrophy, with thickening of the heart muscle.
These cardiac abnormalities cause a right to left cardiac shunt. This means blood bypasses the child’s lungs. Blood bypassing the lungs does not become oxygenated. Deoxygenated blood entering the systemic circulation causes cyanosis. The degree to which this happens is related mostly to the severity of the patients pulmonary stenosis.
Risk Factors
- Rubella infection
- Increased age of the mother (over 40 years)
- Alcohol consumption in pregnancy
- Diabetic mother
Investigations
As with all structural congenital cardiac abnormalities, an echocardiogram is the investigation of choice for establishing the diagnosis. During the echocardiogram, the machine can produce coloured pictures that demonstrate the direction of flow of blood. This is called doppler flow studies. This is useful in assessing the severity of the abnormality and shunt.
A chest xray may show the characteristic “boot shaped” heart due to right ventricular thickening. This not particularly useful diagnostically except during medical exams.
Presentation
Most cases are picked up before the child is born during the antenatal scans. Additionally, an ejection systolic murmur caused by the pulmonary stenosis may be heard on the newborn baby check.
Severe cases will present with heart failure before one year of age. In milder cases, they can present as older children once they start to develop signs and symptoms of heart failure.
Signs and Symptoms
- Cyanosis (blue discolouration of the skin due to low oxygen saturations)
- Clubbing
- Poor feeding
- Poor weight gain
- Ejection systolic murmur heard loudest in the pulmonary area (second intercostal space, left sternal border)
- “Tet spells”
Tet Spells
“Tet Spells” are intermittent symptomatic periods where the right to left shunt becomes temporarily worsened, precipitating a cyanotic episode. This happens when the pulmonary vascular resistance increases or the systemic resistance decreases. For example, if the child is physically exerting themselves they are generating a lot of carbon dioxide. Carbon dioxide is a vasodilator that causes systemic vasodilation and therefore reduces the systemic vascular resistance. Blood flow will choose the path of least resistance, so blood will be pumped from the right ventricle to the aorta rather than the pulmonary vessels, bypassing the lungs.
These episodes may be precipitated by waking, physical exertion or crying. The child will become irritable, cyanotic and short of breath. Severe spells can lead to reduced consciousness, seizures and potentially death.
Tet Spell Treatment Options
Older children may squat when a tet spell occurs. Younger children can be positioned with their knees to their chest. Squatting increases the systemic vascular resistance. This encourages blood to enter the pulmonary vessels.
Any medical management of a tet spell should involve an experienced paediatrician, as they can be potentially life threatening.
- Supplementary oxygen is essential in hypoxic children as hypoxia can be fatal.
- Beta blockers can relax the right ventricle and improve flow to the pulmonary vessels.
- IV fluids can increase pre-load, increasing the volume of blood flowing to the pulmonary vessels.
- Morphine can decrease respiratory drive, resulting in more effective breathing.
- Sodium bicarbonate can buffer any metabolic acidosis that occurs.
- Phenylephrine infusion can increase systemic vascular resistance.
Management and Prognosis
In neonates, a prostaglandin infusion can be used to maintain the ductus arteriosus. This allows blood to flow from the aorta back to the pulmonary arteries.
Total surgical repair by open heart surgery is the definitive treatment, however mortality from surgery is around 5%.
Prognosis depends on the severity, however it is poor without treatment. With corrective surgery, 90% of patients will live into adulthood.
Last updated July 2019
