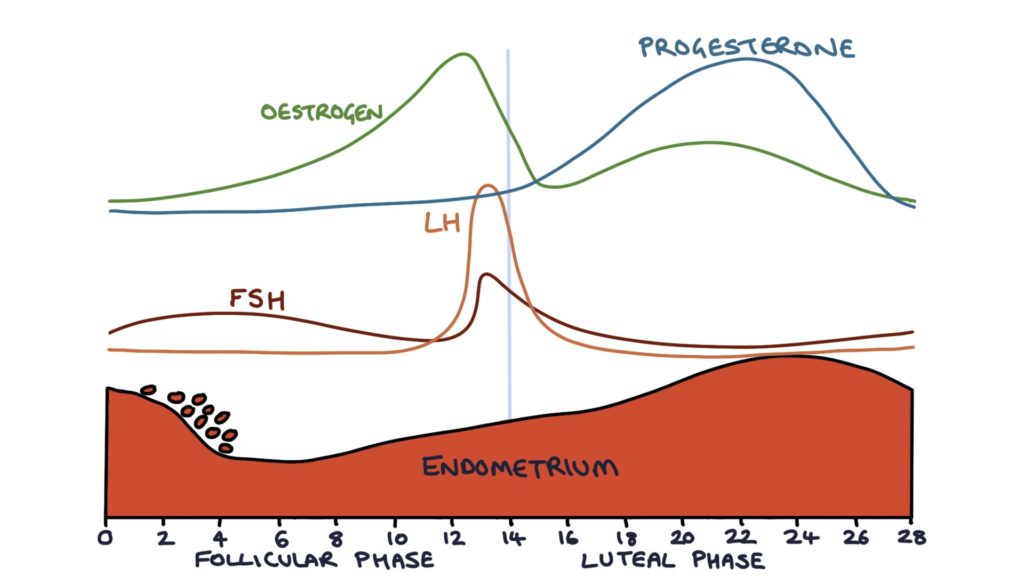
The menstrual cycle consists of two phases: the follicular phase and the luteal phase. The follicular phase is from the start of menstruation to the moment of ovulation (the first 14 days in a 28-day cycle). The luteal phase is from the moment of ovulation to the start of menstruation (the final 14 days of the cycle).
The Follicular Phase
From puberty, the ovaries have a finite number of cells that have the potential to develop into eggs. These cells are called oocytes. Granulosa cells surround the oocytes, forming structures called follicles.
Follicles go through four key stages of development in the ovaries:
- Primordial follicles
- Primary follicles
- Secondary follicles
- Antral follicles (also known as Graafian follicles)
The process of primordial follicles maturing into primary and secondary follicles is always occurring, independent of the menstrual cycle. Once the follicles reach the secondary follicle stage, they develop the receptors for follicle stimulating hormone (FSH). Further development after the secondary follicle stage requires stimulation from FSH.
At the start of the menstrual cycle, FSH stimulates further development of the secondary follicles. As the follicles grow, the granulosa cells that surround them secrete increasing amounts of oestradiol (oestrogen). The oestradiol has a negative feedback effect on the pituitary gland, reducing the quantity of LH and FSH produced. The rising oestrogen also causes the cervical mucus to become more permeable, allowing sperm to penetrate the cervix around the time of ovulation.
One of the follicles will develop further than the others and become the dominant follicle. Luteinising hormone (LH) spikes just before ovulation, causing the dominant follicle to release the ovum (an unfertilised egg) from the ovary. Ovulation happens 14 days before the end of the menstrual cycle, for example, day 14 of a 28-day cycle, or day 16 of a 30-day cycle.
The Luteal Phase
After ovulation, the follicle that released the ovum collapses and becomes the corpus luteum. The corpus luteum secretes high levels of progesterone, which maintains the endometrial lining. This progesterone also causes the cervical mucus to become thick and no longer penetrable. The corpus luteum also secretes a small amount of oestrogen.
When fertilisation occurs, the syncytiotrophoblast of the embryo secretes human chorionic gonadotrophin (HCG). HCG maintains the corpus luteum. Without hCG, the corpus luteum degenerates. Pregnancy tests check for hCG to confirm a pregnancy.
When there is no fertilisation of the ovum, and no production of hCG, the corpus luteum degenerates and stops producing oestrogen and progesterone. This fall in oestrogen and progesterone causes the endometrium to break down and menstruation to occur. Additionally, the stromal cells of the endometrium release prostaglandins. Prostaglandins encourage the endometrium to break down and the uterus to contract. Menstruation starts on day 1 of the menstrual cycle. The negative feedback from oestrogen and progesterone on the hypothalamus and pituitary gland ceases, allowing the levels of LH and FSH to begin to rise, and the cycle to restart.
Menstruation
Menstruation involves the superficial and middle layers of the endometrium separating from the basal layer. The tissue is broken down inside the uterus, and released via the cervix and vagina. The release of fluid containing blood from the vagina lasts 1 – 8 days.
Last updated April 2020
