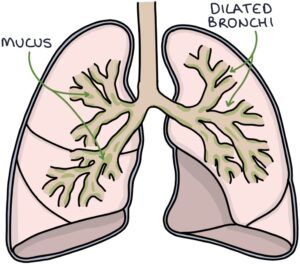
Bronchiectasis involves permanent dilation of the bronchi, the large airways that transport air to the lungs. Sputum collects and organisms grow in the wide tubes, resulting in a chronic cough, continuous sputum production and recurrent infections.
Bronchiectasis results from damage to the airways. Potential causes of this damage include:
- Idiopathic (no apparent cause)
- Pneumonia
- Whooping cough (pertussis)
- Tuberculosis
- Alpha-1-antitrypsin deficiency
- Connective tissue disorders (e.g., rheumatoid arthritis)
- Cystic fibrosis
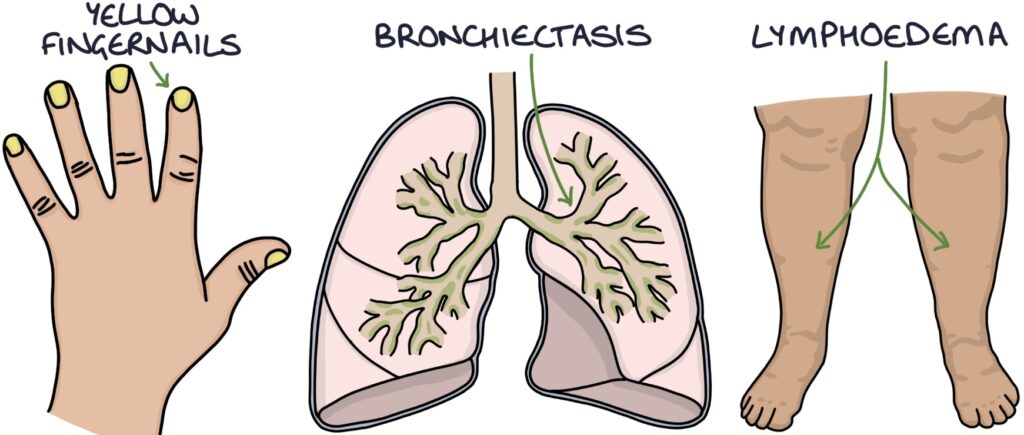
- Yellow nail syndrome
TOM TIP: Yellow nail syndrome is characterised by yellow fingernails, bronchiectasis and lymphoedema. Patients are stable and have good clinical signs, making it a good choice for OSCEs. As it is rare, examiners will score high marks if you can combine these features and name the diagnosis.
Symptoms
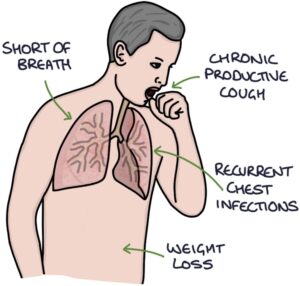
Key presenting symptoms are:
- Shortness of breath
- Chronic productive cough
- Recurrent chest infections
- Weight loss
Signs
Signs of bronchiectasis on examination include:
- Sputum pot by the bedside
- Oxygen therapy (if needed)
- Weight loss (cachexia)
- Finger clubbing
- Signs of cor pulmonale (e.g., raised JVP and peripheral oedema)
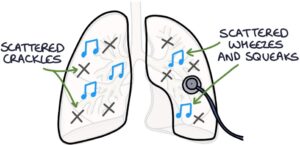
- Scattered crackles throughout the chest that change or clear with coughing
- Scattered wheezes and squeaks
Investigations
Sputum culture is used to identify colonising and infective organisms. The most common infective organisms are:
- Haemophilus influenza
- Pseudomonas aeruginosa
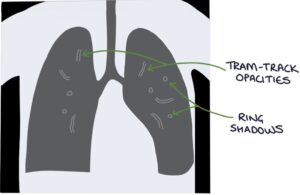
Chest x-ray findings include:
- Tram-track opacities (parallel markings of a side-view of the dilated airway)
- Ring shadows (dilated airways seen end-on)
High-resolution CT (HRCT) is the test of choice for establishing the diagnosis.
Management
General management involves:
- Vaccines (e.g., pneumococcal and influenza)
- Respiratory physiotherapy to help clear sputum
- Pulmonary rehabilitation
- Long-term antibiotics (e.g., azithromycin) for frequent exacerbations (e.g., 3 or more per year)
- Inhaled colistin for Pseudomonas aeruginosa colonisation
- Long-acting bronchodilators may be considered for breathlessness
- Long-term oxygen therapy in patients with reduced oxygen saturation
- Surgical lung resection may be considered for specific areas of disease
- Lung transplant is an option for end-stage disease
Infective exacerbations require:
- Sputum culture (before antibiotics)
- Extended courses of antibiotics, usually 7–14 days
- Ciprofloxacin is the usual choice for exacerbations caused by Pseudomonas aeruginosa
TOM TIP: The key features to remember with bronchiectasis are finger clubbing, diagnosis by HRCT, Pseudomonas colonisation and extended courses of 7-14 days of antibiotics for exacerbations.
Last updated September 2023
