Diabetic retinopathy involves damage to the retinal blood vessels due to prolonged high blood sugar levels.
Pathophysiology
Hyperglycaemia (high blood sugar) damages the retinal small vessels and endothelial cells.
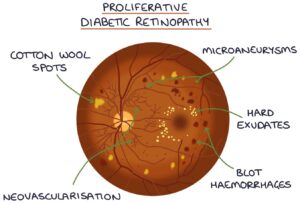
Increased vascular permeability leads to leaking blood vessels, blot haemorrhages and hard exudates. Hard exudates are yellow-white deposits of lipids and proteins in the retina.
Damage to the blood vessel walls leads to microaneurysms and venous beading. Microaneurysms are small bulges in the blood vessel walls. Venous beading is where the walls of the veins are no longer straight and parallel and look more like a string of beads or sausages.
Damage to nerve fibres in the retina causes fluffy white patches called cotton wool spots to form on the retina.
Intraretinal microvascular abnormalities (IRMA) refer to dilated and tortuous capillaries in the retina. These can act as a shunt between the arterial and venous vessels in the retina.
Neovascularisation involves the release of growth factors in the retina, stimulating new blood vessel development.
Grading
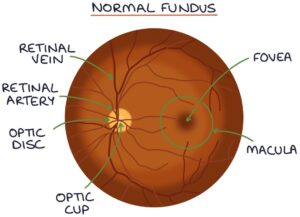
Diabetic retinopathy is graded based on the findings on fundus examination:
- Background – microaneurysms, retinal haemorrhages, hard exudates and cotton wool spots
- Pre-proliferative – venous beading, multiple blot haemorrhages and intraretinal microvascular abnormality (IMRA)
- Proliferative – neovascularisation and vitreous haemorrhage
Diabetic maculopathy also exists separately and involves:
- Exudates within the macula
- Macular oedema
TOM TIP: The main distinction is between non-proliferative (which includes background and pre-proliferative) and proliferative diabetic retinopathy. The key feature of proliferative diabetic retinopathy is the development of new blood vessels (neovascularisation).
Complications
- Vision loss
- Retinal detachment
- Vitreous haemorrhage (bleeding into the vitreous humour)
- Rubeosis iridis (new blood vessel formation in the iris) – this can lead to neovascular glaucoma
- Optic neuropathy
- Cataracts
Management
Non-proliferative diabetic retinopathy requires close monitoring and careful diabetic control.
Treatment options for proliferative diabetic retinopathy are:
- Pan-retinal photocoagulation (PRP) – extensive laser treatment across the retina to suppress new vessels
- Anti-VEGF medications by intravitreal injection
- Surgery (e.g., vitrectomy) may be required in severe disease
An intravitreal implant containing dexamethasone is an option for macular oedema.
TOM TIP: Look up pictures of a retina treated with pan-retinal photocoagulation so you can spot it in exams.
Last updated October 2023
