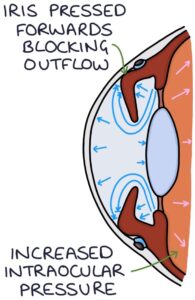
Acute angle closure glaucoma occurs when the iris bulges forward and seals off the trabecular meshwork from the anterior chamber, preventing aqueous humour from draining and leading to a continual increase in intraocular pressure. The pressure builds in the posterior chamber, pushing the iris forward and exacerbating the angle closure.
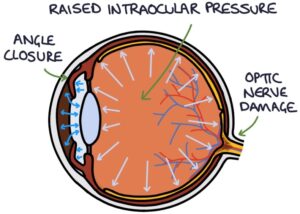
It is an ophthalmological emergency requiring rapid treatment to prevent permanent vision loss.
Risk Factors
Risk factors for acute angle-closure glaucoma include:
- Increasing age
- Family history
- Female (four times more likely than males)
- Chinese and East Asian ethnic origin
- Shallow anterior chamber
TOM TIP: Note the difference in risk factors between angle-closure and open-angle glaucoma, particularly in ethnic origin. Open-angle glaucoma is more common in black people, while angle-closure glaucoma is rare in this group. If an exam question mentions ethnic origin, it is probably relevant as a risk factor.
Certain medications can precipitate acute angle-closure glaucoma:
- Adrenergic medications (e.g., noradrenaline)
- Anticholinergic medications (e.g., oxybutynin and solifenacin)
- Tricyclic antidepressants (e.g., amitriptyline), which have anticholinergic effects
Presentation
A typical patient with acute angle-closure glaucoma presents appearing generally unwell, with a short history of:
- Severely painful red eye
- Blurred vision
- Halos around lights
- Associated headache, nausea and vomiting
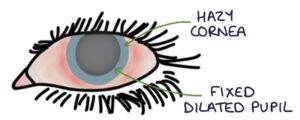
Signs on examination include:
- Red eye
- Hazy cornea
- Decreased visual acuity
- Mid-dilated pupil
- Fixed-size pupil
- Hard eyeball on gentle palpation
Initial Management
Acute angle-closure glaucoma requires immediate admission. Measures while waiting for an ambulance are:
- Lying the patient on their back without a pillow
- Pilocarpine eye drops (2% for blue and 4% for brown eyes)
- Acetazolamide 500 mg orally
- Analgesia and an antiemetic, if required
Pilocarpine acts on the muscarinic receptors in the sphincter muscles in the iris and causes pupil constriction (it is a miotic agent). It also causes ciliary muscle contraction. These two effects open up the pathway for the flow of aqueous humour from the ciliary body, around the iris and into the trabecular meshwork.
Acetazolamide is a carbonic anhydrase inhibitor that reduces the production of aqueous humour.
Secondary Care Management
Specialist medical options include:
- Pilocarpine eye drops
- Acetazolamide (oral or intravenous)
- Hyperosmotic agents (e.g., intravenous mannitol) increase the osmotic gradient between the blood and the eye
- Timolol is a beta blocker that reduces the production of aqueous humour
- Dorzolamide is a carbonic anhydrase inhibitor that reduces the production of aqueous humour
- Brimonidine is a sympathomimetics that reduces aqueous humour production and increases uveoscleral outflow
Laser iridotomy is usually required as a definitive treatment. This involves making a hold in the iris using a laser, which allows the aqueous humour to flow directly from the posterior chamber to the anterior chamber. This relieves the pressure pushing the iris forward against the cornea and opens the pathway for the aqueous humour to drain.
Last updated October 2023
