Clostridium difficile (“C. diff”) is a gram-positive, rod-shaped, anaerobic bacteria.
Infection is associated with repeated use of antibiotics, proton-pump inhibitors (e.g., omeprazole) and healthcare settings.
C. difficile produces spores, which are released in faeces. The spores can survive on contaminated surfaces and hands, helping it spread to others.
It may colonise the intestines without causing any symptoms or issues. When antibiotics interrupt the normal intestinal microbiome, C. difficile can proliferate and get out of control. It can produce toxins, particularly toxin A (enterotoxin) and toxin B (cytotoxin), which cause symptoms and complications.
Antibiotics
The antibiotics most associated with C. difficile start with the letter C:
- Clindamycin
- Ciprofloxacin (and other fluoroquinolones)
- Cephalosporins
- Carbapenems (e.g., meropenem)
Presentation
Colonisation is usually asymptomatic.
Infection presents with diarrhoea, nausea and abdominal pain.
Severe infection with colitis can present with:
- Dehydration
- Systemic symptoms (e.g., fever, tachycardia and hypotension)
Diagnosis
Diagnosis is based on stool samples. Stools can be tested for:
- C. difficile antigen (specifically glutamate dehydrogenase)
- A and B toxins (by PCR or enzyme immunoassay)
The antigen test shows whether C. difficile is present but not whether it is producing toxins. The antigen is the initial screening test and is followed up with tests for toxins if C. difficile is identified.
Management
Management is with supportive care and oral antibiotics. The options are:
- Oral vancomycin (first-line)
- Oral fidaxomicin (second-line)
Patients need to be isolated until 48 hours after the last episode of diarrhoea. There is a high recurrence rate.
Faecal microbiota transplantation is an option for recurrent cases. The stool microbiome from a donor is transferred to the patient via capsules, colonoscopy or enema.
Complications
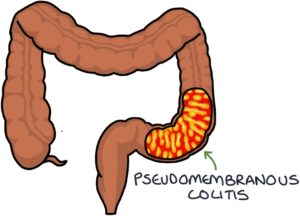
Pseudomembranous colitis is characterised by inflammation in the large intestine, with yellow/white plaques that form pseudomembranes on the inner surface of the bowel wall. It is seen during a colonoscopy and confirmed with biopsies to examine the histology.
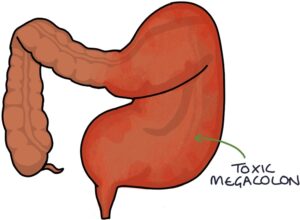
Toxic megacolon is a complication of severe inflammation in the large intestine and involves dilation of the colon. Patients with toxic megacolon are very unwell and have a high risk of bowel rupture. Treatment involves supportive care and surgical resection of the affected bowel.
Additional complications include bowel perforation and sepsis.
Last updated July 2023
