Osteomalacia is a condition where defective bone mineralisation causes “soft” bones. Osteo– means bone, and –malacia means soft. It results from insufficient vitamin D. The same process in children causes rickets.
Simplified Pathophysiology
Vitamin D is a hormone the skin creates in response to sunlight. It is also obtained in limited amounts from food. It is vital in regulating bone mineralisation, hormone secretion and immune function. Low vitamin D is very common.
Vitamin D is created from cholesterol by the skin in response to UV radiation. Patients with darker skin require more prolonged sun exposure to generate the same vitamin D. It is also obtained from food as a fat-soluble vitamin. A regular diet does not contain enough vitamin D to compensate for reduced sun exposure.
Patients with malabsorption disorders (e.g., inflammatory bowel disease) are at higher risk of vitamin D deficiency. Patients with chronic kidney disease are also at higher risk of vitamin D deficiency as the kidneys help convert vitamin D into its active form.
Vitamin D is essential in calcium and phosphate absorption in the intestines and reabsorption in the kidneys. It is also responsible for regulating bone turnover and promoting bone reabsorption to increase the serum calcium level.
Inadequate vitamin D leads to low serum calcium and phosphate. Since calcium and phosphate are required for the construction of bone, low levels result in defective bone mineralisation and osteomalacia.
Low calcium leads to increased parathyroid hormone (PTH) secretion by the parathyroid glands (secondary hyperparathyroidism). Increased parathyroid hormone promotes calcium reabsorption from the bones, further impairing bone mineralisation.
TOM TIP: Most guidelines recommend against testing asymptomatic patients with risk factors for deficiency for their vitamin D level. They should be advised to take maintenance vitamin D without needing a test.
Presentation
Patients with vitamin D deficiency and osteomalacia may not have any symptoms. Typical symptoms include:
- Fatigue
- Bone pain
- Muscle weakness
- Muscle aches
- Pathological or abnormal fractures
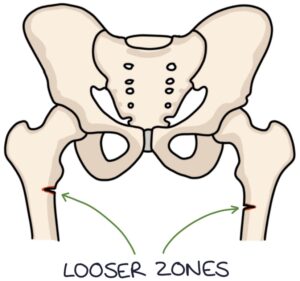
Looser zones are fragility fractures that go partially through the bone.
TOM TIP: Consider vitamin D deficiency risk factors in your exams and clinical practice. Patients with osteomalacia are likely to have risk factors such as darker skin, low exposure to sunlight, living in colder climates and spending most of their time indoors.
Investigations
Serum 25-hydroxyvitamin D is the laboratory investigation for vitamin D:
- Less than 25 nmol/L – vitamin D deficiency
- 25 to 50 nmol/L – vitamin D insufficiency
Other laboratory investigation results include:
- Low serum calcium
- Low serum phosphate
- High serum alkaline phosphatase
- High parathyroid hormone (secondary hyperparathyroidism)
Imaging investigations include:
- X-rays may show osteopenia (more radiolucent bones)
- DEXA scan shows low bone mineral density
Treatment
Treatment is with colecalciferol (vitamin D₃). There are various loading regimes (e.g., for patients with symptoms) suggested by the NICE clinical knowledge summaries (2022), for example:
- 50,000 IU once weekly for 6 weeks
- 4000 IU daily for 10 weeks
A maintenance dose of 800-2000 IU per day is continued following the loading regime (or as the initial treatment in patients that do not require rapid treatment.
NICE CKS (2022) recommend checking the serum calcium within a month of the loading regime. It may be:
- Low in calcium deficiency
- High in primary hyperparathyroidism (previously masked by the vitamin D deficiency)
- High in other conditions that cause hypercalcaemia, such as cancer, sarcoidosis or tuberculosis
Last updated September 2023
