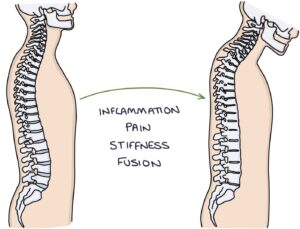
Ankylosing spondylitis (AS) is an inflammatory condition affecting the axial skeleton (mainly the spine and sacroiliac joints), causing progressive stiffness and pain. It is also known as axial spondyloarthritis. It is part of the seronegative spondyloarthropathy group of conditions, also including psoriatic arthritis and reactive arthritis.
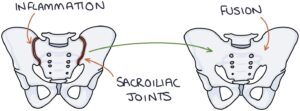
The main affected joints are the sacroiliac joints and the vertebral column joints. Inflammation causes pain and stiffness in these joints. It can progress to spine and sacroiliac joint fusion.
There is a strong link with the HLA-B27 gene. Around 90% of AS patients have the HLA-B27 gene. It is thought that less than 10% of people with the gene will get AS. It is more common in men (but women can also be affected).
Presentation
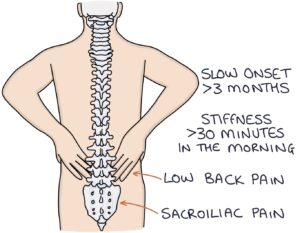
The typical presentation is a young adult male in their 20s. Symptoms develop gradually over at least three months.
The main presenting features are
- Pain and stiffness in the lower back
- Sacroiliac pain (in the buttock region)
The pain and stiffness is worse with rest and improves with movement. The pain worsens at night and in the morning and may wake them. The stiffness takes at least 30 minutes to improve in the morning. Symptoms improve with activity and worsen with rest.
Additional symptoms and problems include:
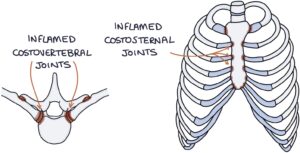
- Chest pain related to the costovertebral and sternocostal joints
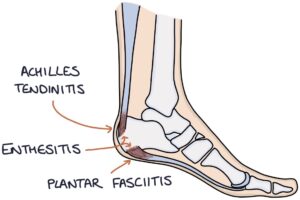
- Enthesitis (inflammation of the entheses, where tendons or ligaments insert into bone)
- Dactylitis (inflammation of the entire finger)
- Vertebral fractures (presenting with sudden-onset new neck or back pain)
- Shortness of breath relating to restricted chest wall movement)
Associations
There is a long list of associated conditions. The key ones can be remembered with the 5 As mnemonic:
- A – Anterior uveitis
- A – Aortic regurgitation
- A – Atrioventricular block (heart block)
- A – Apical lung fibrosis (fibrosis of the upper lobes of the lungs)
- A – Anaemia of chronic disease
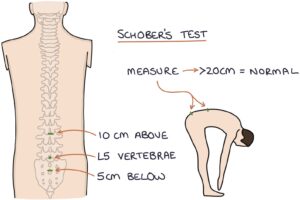
Schober’s Test
Schober’s test assesses spinal mobility. With the patient standing straight, the L5 vertebra is located, and a point is marked 10cm above and 5cm below this level (15cm apart). Then the patient bends forward as far as possible, and the distance between the points is measured. A length of less than 20cm indicates a restriction in lumbar movement and helps support a diagnosis of ankylosing spondylitis.
Investigations
Key investigations include:
- Inflammatory markers (e.g., CRP and ESR) may rise with disease activity
- HLA B27 genetic testing
- X-ray of the spine and sacrum
- MRI of the spine can show bone marrow oedema early in the disease before there are any xray changes
X-ray Changes
A “bamboo spine” is the typical x-ray finding in the later stages of ankylosing spondylitis, where there is fusion of the sacroiliac and spinal joints.
X-rays in ankylosing spondylitis can show:
- Squaring of the vertebral bodies
- Subchondral sclerosis and erosions
- Syndesmophytes (areas of bone growth where the ligaments insert into the bone)
- Ossification of the ligaments, discs and joints (these structures start turning into bone)
- Fusion of the facet, sacroiliac and costovertebral joints
Management
The rheumatology multidisciplinary team will manage patients. Treatment aims to control symptoms and preserve function.
Medical management may involve:
- Non-steroidal anti-inflammatory drugs (NSAIDs) are first-line
- Anti-TNF medications are second-line (e.g., adalimumab, etanercept or infliximab)
- Secukinumab or ixekizumab are third-line (monoclonal antibodies against interleukin-17)
- Upadacitinib is another third-line option (JAK inhibitor)
Intra-articular steroid injections may be considered for specific joints.
Additional management:
- Physiotherapy
- Exercise and mobilisation
- Avoiding smoking
- Bisphosphonates for osteoporosis
- Surgery is occasionally required for severe joint deformity
Last updated August 2023
