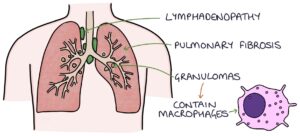
Sarcoidosis is a chronic granulomatous disorder. Granulomas are inflammatory nodules full of macrophages. The cause of these granulomas is unknown.
It is usually associated with respiratory symptoms but has many extra-pulmonary manifestations, such as erythema nodosum and lymphadenopathy. Symptoms can vary dramatically from asymptomatic to severe or life-threatening.
Epidemiology
Sarcoidosis can affect anyone. It seems to be slightly more common in:
- Aged 20-39 or around 60
- Women
- Black ethnic origin
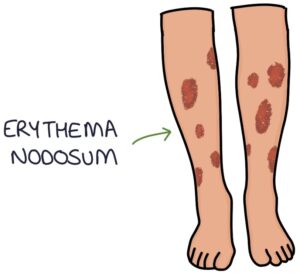
TOM TIP: The typical MCQ exam patient is a 20-40 year old black female presenting with a dry cough and shortness of breath. They may have nodules on their shins, suggesting erythema nodosum.
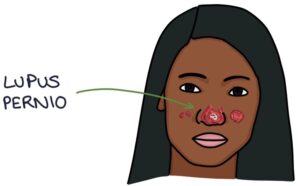
Skin Features
Less than half of patients with sarcoidosis have skin involvement. However, these findings are worth remembering for exams.
Erythema nodosum is characterised by nodules of inflamed subcutaneous fat on the shins. Inflammation of fat is called panniculitis. Erythema nodosum presents as raised, red, tender, painful, subcutaneous nodules across both shins. Over time the nodules settle and appear as bruises. There are many causes of erythema nodosum.
Lupus pernio is specific to sarcoidosis and presents with raised purple skin lesions, often on the cheeks and nose.
Organs Affected
Sarcoidosis can affect almost any organ in the body. The lungs are most commonly affected (in over 90% of patients), so respiratory physicians usually manage sarcoidosis.
Lungs:
- Mediastinal lymphadenopathy
- Pulmonary fibrosis
- Pulmonary nodules
Systemic Symptoms:
- Fever
- Fatigue
- Weight loss
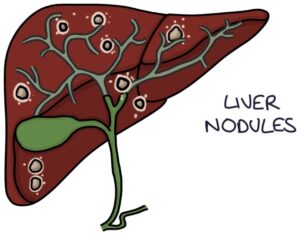
Liver:
- Liver nodules
- Cirrhosis
- Cholestasis
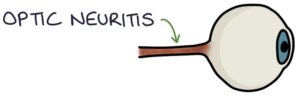
Eyes:
- Uveitis
- Conjunctivitis
- Optic neuritis


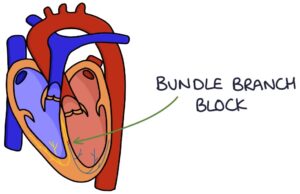
Heart:
- Bundle branch block
- Heart block
- Myocardial muscle involvement
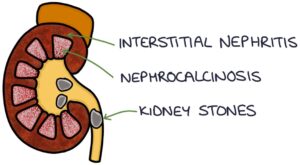
Kidneys:
- Kidney stones (due to hypercalcaemia)
- Nephrocalcinosis
- Interstitial nephritis
Central nervous system:
- Nodules
- Pituitary involvement (diabetes insipidus)
- Encephalopathy
Peripheral Nervous System:
- Facial nerve palsy
- Mononeuritis multiplex
Bones:
- Arthralgia
- Arthritis
- Myopathy
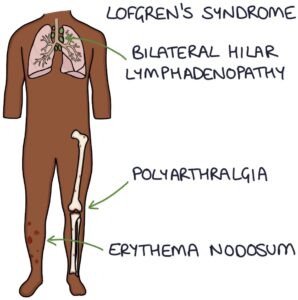
Lofgren’s Syndrome
Lofgren’s syndrome refers to a specific presentation of sarcoidosis with a classic triad of symptoms:
- Erythema nodosum
- Bilateral hilar lymphadenopathy
- Polyarthralgia (joint pain in multiple joints)
Differential Diagnosis
The top differentials for the varied presenting features of sarcoidosis are:
- Tuberculosis
- Lymphoma
- Hypersensitivity pneumonitis
- HIV
- Toxoplasmosis
- Histoplasmosis
Blood Tests
The blood test findings to remember are:
- Raised angiotensin-converting enzyme (ACE) (often used as a screening test)
- Raised calcium (hypercalcaemia)
Imaging
Various imaging investigations may be performed:
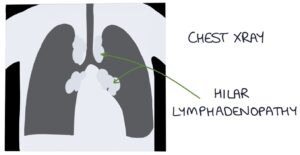
- Chest x-ray may show hilar lymphadenopathy
- High-resolution CT scanning may show hilar lymphadenopathy and pulmonary nodules
- MRI can show central nervous system involvement
- PET scan can show active inflammation in affected areas
Histology
Histology helps establish the diagnosis, often by bronchoscopy with an ultrasound-guided biopsy of mediastinal lymph nodes. Histology characteristically shows non-caseating granulomas with epithelioid cells.
Other Tests
Other tests may be used to determine which organs are affected:
- U&Es for kidney involvement
- Urine albumin-creatinine ratio to look for proteinuria
- LFTs for liver involvement
- Ophthalmology assessment for eye involvement
- ECG and echocardiogram for heart involvement
- Ultrasound for liver and kidney involvement
Management
Conservative management is considered in patients with no or mild symptoms.
Oral steroids (for 6-24 months) are usually first-line where treatment is required. Bisphosphonates protect against osteoporosis whilst on long-term steroids.
Methotrexate is a second-line option.
Lung transplant is rarely required in severe pulmonary disease.
Prognosis
Sarcoidosis spontaneously resolves in around half of patients, usually within two years. In some patients, it progresses to pulmonary fibrosis and pulmonary hypertension. Overall mortality is less than 10%.
Last updated June 2023
