Keratitis refers to inflammation of the cornea. There are many causes of keratitis:
- Viral infection (e.g., herpes simplex)
- Bacterial infection (e.g., Pseudomonas or Staphylococcus)
- Fungal infection (e.g., Candida or Aspergillus)
- Contact lens-induced acute red eye (CLARE)
- Exposure keratitis, caused by inadequate eyelid coverage (e.g., ectropion)
Herpes simplex virus (HSV) infection is the most common cause of keratitis and is called herpes simplex keratitis. HSV can cause inflammation in any part of the eye but most commonly affects the epithelial layer of the cornea.
Herpes simplex keratitis can be primary or recurrent. Recurrence is caused by the virus travelling to the trigeminal ganglion, where it becomes latent (dormant) and can reactivate later.
Herpes simplex keratitis usually affects only the epithelial layer of the cornea. Inflammation of the stroma (the layer between the epithelium and endothelium) is called stromal keratitis. This is associated with complications such as stromal necrosis, vascularisation and scarring and can lead to corneal blindness.
Presentation
Primary infection often involves mild symptoms of blepharoconjunctivitis (inflammation of the eyelid margins and conjunctiva).
Recurrent infection may present with:
- Painful red eye
- Photophobia
- Vesicles (fluid-filled blisters)
- Foreign body sensation
- Watery discharge
- Reduced visual acuity
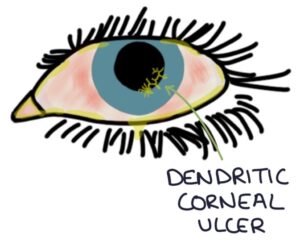
Slit lamp examination is required to diagnose keratitis. Fluorescein staining shows a dendritic corneal ulcer. Dendritic describes the branching appearance of the ulcer.
Corneal scrapings can be used for viral testing.
Management
Patients should be referred for urgent assessment and management by an ophthalmologist.
Specialist management involves topical or oral antivirals (e.g., aciclovir or ganciclovir).
Corneal transplant is an option to treat permanent scarring and vision loss after keratitis.
Last updated October 2023
