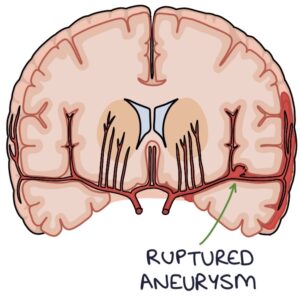
Subarachnoid haemorrhage involves bleeding in the subarachnoid space, where the cerebrospinal fluid is located, between the pia mater and the arachnoid membrane. This is usually the result of a ruptured cerebral aneurysm.
Subarachnoid haemorrhage has a very high mortality (around 30%) and morbidity, making it essential not to miss.
Risk Factors
It is more common in:
- Aged 45 to 70
- Women
- Black ethnic origin
General risk factors include:
- Hypertension
- Smoking
- Excessive alcohol intake
Subarachnoid haemorrhage is particularly associated with:
- Family history
- Cocaine use
- Sickle cell anaemia
- Connective tissue disorders (e.g., Marfan syndrome or Ehlers-Danlos syndrome)
- Neurofibromatosis
- Autosomal dominant polycystic kidney disease
Presentation
The typical history is a sudden-onset occipital headache during strenuous activity, such as heavy lifting or sex. The sudden and severe onset leads to the “thunderclap headache” description. It may feel like being struck over the back of the head.
Other important features include:
- Neck stiffness
- Photophobia
- Vomiting
- Neurological symptoms (e.g., visual changes, dysphasia, focal weakness, seizures and reduced consciousness)
Investigations
CT head is the first-line investigation. Blood will cause hyper-attenuation in the subarachnoid space. However, a normal CT head does not exclude a subarachnoid haemorrhage. CT is less reliable more than 6 hours after the start of symptoms.
Lumbar puncture is considered after a normal CT head. The NICE guidelines (2022) recommend waiting at least 12 hours after the symptoms start before performing a lumbar puncture, as it takes time for the bilirubin to accumulate in the cerebrospinal fluid (CSF). With a subarachnoid haemorrhage, a CSF sample will show:
- Raised red cell count (a decreasing red cell count on successive bottles may be due to a traumatic procedure)
- Xanthochromia (a yellow colour to the CSF caused by bilirubin)
CT angiography is used after confirming the diagnosis to locate the source of the bleeding.
Management
Patients should be managed by a specialist neurosurgical unit. Patients with reduced consciousness may require intubation and ventilation. Supportive care involves a multi-disciplinary team during the initial stages and recovery.
Surgical intervention may be used to treat aneurysms. The aim is to repair the vessel and prevent re-bleeding. This can be done by endovascular coiling, which involves inserting a catheter into the arterial system (an endovascular approach), placing platinum coils in the aneurysm and sealing it off from the artery. An alternative is neurosurgical clipping, which involves cranial surgery and putting a clip on the aneurysm to seal it.
Nimodipine is a calcium channel blocker used to prevent vasospasm. Vasospasm is a common complication following a subarachnoid haemorrhage, resulting in brain ischaemia.
Management of Complications
Hydrocephalus refers to increased cerebrospinal fluid, causing expansion of the ventricles. Treatment options include:
- Lumbar puncture
- External ventricular drain (a drain inserted into the brain ventricles to drain CSF)
- Ventriculoperitoneal (VP) shunt (a catheter connecting the ventricles with the peritoneal cavity)
Seizures are treated with anti-epileptic drugs.
Last updated September 2023
