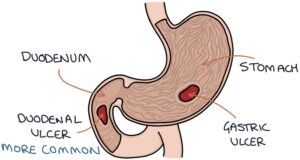
Peptic ulcers involve ulceration of the mucosa of the stomach (gastric ulcer) or the proximal duodenum (duodenal ulcer). Duodenal ulcers are more common.
Pathophysiology
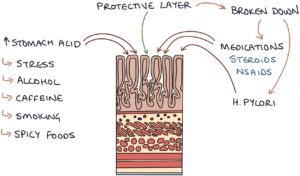
The mucosa, also known as the mucous membrane, is the inner lining of the stomach and duodenum. It secretes mucus that coats the surface and forms a barrier that protects it from the stomach’s contents, particularly stomach acid and digestive enzymes. It secretes bicarbonate into this mucus coating to neutralise the stomach acid.
Factors that disrupt the mucus barrier or increase stomach acid increase the risk of mucosal ulceration.
Risk Factors
The risk key factors that disrupt the mucus barrier are:
- Helicobacter pylori
- Non-steroidal anti-inflammatory drugs (NSAIDs)

The risk key factors that increase stomach acid are:
- Stress
- Alcohol
- Caffeine
- Smoking
- Spicy foods
The risk of bleeding from a peptic ulcer is increased with the use of:
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Aspirin
- Anticoagulants (e.g., DOACs)
- Steroids
- SSRI antidepressants
Presentation
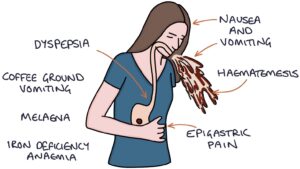
Peptic ulcers present with non-specific symptoms of:
- Epigastric discomfort or pain
- Nausea and vomiting
- Dyspepsia
The signs of upper gastrointestinal bleeding are:
- Haematemesis (vomiting blood)
- Coffee ground vomiting
- Melaena (black, tarry stools)
- Fall in haemoglobin on a full blood count
Chronic microscopic bleeding can lead to iron deficiency anaemia, with low haemoglobin, low mean cell volume (MCV) and low ferritin.
TOM TIP: Eating typically worsens the pain of gastric ulcers. The pain of duodenal ulcers tends to improve immediately after eating, followed by pain 2-3 hours later. Patients with gastric ulcers tend to lose weight due to the fear of pain on eating, whereas with duodenal ulcers, the weight is stable or increases. This helps you differentiate them in your MCQ exams.
Diagnosis
Peptic ulcers can be diagnosed on endoscopy. During endoscopy, a rapid urease test (CLO test) can be performed to check for H. pylori. A biopsy is considered during endoscopy to exclude malignancy.
Management
The core aspects of treating peptic ulcers are:
- Stopping NSAIDs
- Treating H. pylori infections
- Proton pump inhibitors (e.g., lansoprazole or omeprazole)
Repeat endoscopy (at 4-8 weeks) may be performed to ensure the ulcer heals.
Complications
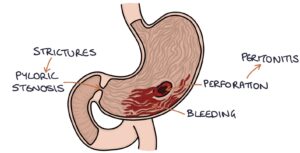
Bleeding from the ulcer is a common and potentially life-threatening complication.
Perforation results in acute abdominal pain and peritonitis, requiring urgent surgical repair (usually laparoscopic).
Scarring and strictures can lead to a narrowing of the exit of the stomach, causing difficulty in emptying the stomach contents. This is known as gastric outlet obstruction and presents with early fullness after eating as well as upper abdominal discomfort, abdominal distention and vomiting, particularly after eating. This may be treated with balloon dilatation during an endoscopy or surgery.
Last updated May 2023
