Coeliac disease is an autoimmune condition triggered by eating gluten. It can develop at any age and is thought to be caused by genetic and environmental factors. There is a link with other autoimmune conditions, particularly type 1 diabetes and thyroid disease.
TOM TIP: Remember for your exams that we test all new cases of type 1 diabetes and autoimmune thyroid disease for coeliac disease, even if they do not have symptoms.
Pathophysiology
In patients with coeliac disease, autoantibodies are created in response to exposure to gluten. These autoantibodies target the epithelial cells of the small intestine, leading to inflammation. These antibodies relate to disease activity and will rise with more active disease and may disappear with effective management. There are three antibodies related to coeliacs (particularly worth remembering the first two):
- Anti-tissue transglutaminase antibodies (anti-TTG)
- Anti-endomysial antibodies (anti-EMA)
- Anti-deamidated gliadin peptide antibodies (anti-DGP)
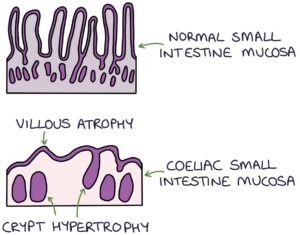
Inflammation affects the small bowel, particularly the jejunum. The surface of the small intestine is covered in projections called villi, which increase the surface area and help with nutrient absorption. Coeliac disease causes atrophy of the intestinal villi, resulting in malabsorption.
It is associated with certain human leukocyte antigen (HLA) genotypes:
- HLA-DQ2
- HLA-DQ8
Presentation
Coeliac disease is often asymptomatic and is under-diagnosed, so have a low threshold for testing for coeliac disease in patients where it is suspected.
Presenting symptoms can include:
- Failure to thrive in young children
- Diarrhoea
- Bloating
- Fatigue
- Weight loss
- Mouth ulcers
Dermatitis herpetiformis is an itchy, blistering skin rash, typically on the abdomen, caused by coeliac disease.
Anaemia occurs secondary to malabsorption and deficiency of iron, B12 or folate.
Rarely coeliac disease can present with neurological symptoms:
- Peripheral neuropathy
- Cerebellar ataxia
- Epilepsy
Diagnosis
The patient must continue eating gluten while being investigated. Antibodies and histology may be normal if the patient is gluten-free.
The first-line blood tests are:
- Total immunoglobulin A levels (to exclude IgA deficiency)
- Anti-tissue transglutaminase antibodies (anti-TTG)
Anti-endomysial antibodies (anti-EMA) are a second-line option where there is doubt (e.g., a borderline result).
TOM TIP: Initial anti-TTG and anti-EMA antibody tests are IgA. Some patients have an IgA deficiency. When you test for these antibodies, it is important to test for total immunoglobulin A levels because if the total IgA level is low, the antibody test will be negative, even in a patient with coeliac disease. In this circumstance, you can test for the IgG version of anti-TTG or anti-EMA antibodies.
Patients with a positive antibody test are referred to a gastroenterologist to confirm the diagnosis by endoscopy and jejunal biopsy. Typical biopsy findings are:
- Crypt hyperplasia
- Villous atrophy
Management
A lifelong gluten-free diet should completely resolve the symptoms. Dietician input may be helpful. Relapse will occur upon consuming gluten. Coeliac antibodies may help monitor the disease.
Complications
If someone with coeliac disease continues eating gluten, even in tiny amounts, it can lead to:
- Nutritional deficiencies
- Anaemia
- Osteoporosis
- Hyposplenism (with immunodeficiency, particularly to encapsulated bacteria such as Streptococcus pneumoniae)
- Ulcerative jejunitis
- Enteropathy-associated T-cell lymphoma (EATL)
- Non-Hodgkin lymphoma
- Small bowel adenocarcinoma
Last updated May 2023
