Definitions
Hyperthyroidism is where there is over-production of the thyroid hormones, triiodothyronine (T3) and thyroxine (T4), by the thyroid gland.
Thyrotoxicosis refers to the effects of an abnormal and excessive quantity of thyroid hormones in the body.
Primary hyperthyroidism is due to thyroid pathology. The thyroid is behaving abnormally and producing excessive thyroid hormone.
Secondary hyperthyroidism is due to pathology in the hypothalamus or pituitary. The pituitary gland produces too much thyroid-stimulating hormone, stimulating the thyroid gland to produce excessive thyroid hormones.
Subclinical hyperthyroidism is where the thyroid hormones (T3 and T4) are normal and thyroid-stimulating hormone (TSH) is suppressed (low). There may be absent or mild symptoms.
Graves’ disease is an autoimmune condition where TSH receptor antibodies cause primary hyperthyroidism. These TSH receptor antibodies, produced by the immune system, stimulate TSH receptors on the thyroid. This is the most common cause of hyperthyroidism.
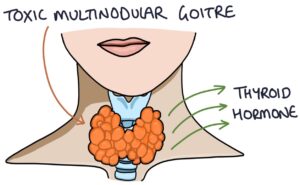
Toxic multinodular goitre (also known as Plummer’s disease) is a condition where nodules develop on the thyroid gland, which are unregulated by the thyroid axis and continuously produce excessive thyroid hormones. It is most common in patients over 50 years.
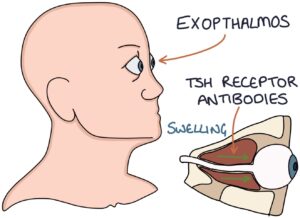
Exophthalmos (also known as proptosis) describes the bulging of the eyes caused by Graves’ disease. Inflammation, swelling and hypertrophy of the tissue behind the eyeballs force them forward, causing them to bulge out of the sockets.
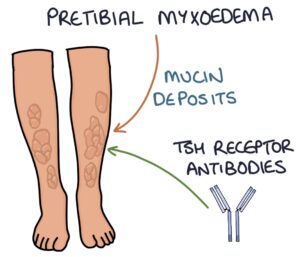
Pretibial myxoedema is a skin condition caused by deposits of glycosaminoglycans under the skin on the anterior aspect of the leg (the pre-tibial area). It gives the skin a discoloured, waxy, oedematous appearance over this area. It is specific to Grave’s disease and is a reaction to TSH receptor antibodies.
Goitre refers to the neck lump caused by swelling of the thyroid gland.
Causes
The causes of hyperthyroidism can be remembered with the “GIST” mnemonic:
- G – Graves’ disease
- I – Inflammation (thyroiditis)
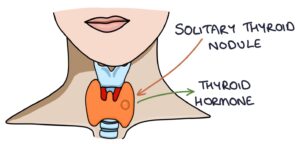
- S – Solitary toxic thyroid nodule
- T – Toxic multinodular goitre
Thyroiditis (thyroid gland inflammation) often causes an initial period of hyperthyroidism, followed by under-activity of the thyroid gland (hypothyroidism). The causes of thyroiditis include:
- De Quervain’s thyroiditis
- Hashimoto’s thyroiditis
- Postpartum thyroiditis
- Drug-induced thyroiditis
Presentation
The features that are universal to all causes of hyperthyroidism include:
- Anxiety and irritability
- Sweating and heat intolerance
- Tachycardia
- Weight loss
- Fatigue
- Insomnia
- Frequent loose stools
- Sexual dysfunction
- Brisk reflexes on examination
Graves’ disease has specific features relating to the presence of TSH receptor antibodies:
- Diffuse goitre (without nodules)
- Graves’ eye disease, including exophthalmos
- Pretibial myxoedema
- Thyroid acropachy (hand swelling and finger clubbing)
Nodules may be palpable within a swollen thyroid gland (goitre) in patients with toxic multinodular goitre.
Solitary Toxic Thyroid Nodule
A solitary toxic thyroid nodule is where a single abnormal thyroid nodule acts alone to release excessive thyroid hormone. The nodules are usually benign adenomas. Treatment involves surgical removal of the nodule.
De Quervain’s Thyroiditis
De Quervain’s thyroiditis, also known as subacute thyroiditis, is a condition causing temporary inflammation of the thyroid gland. There are three phases:
- Thyrotoxicosis
- Hypothyroidism
- Return to normal
The initial thyrotoxic phase involves:
- Excessive thyroid hormones
- Thyroid swelling and tenderness
- Flu-like illness (fever, aches and fatigue)
- Raised inflammatory markers (CRP and ESR)
It is a self-limiting condition, and supportive treatment is usually all that is necessary. This may involve:
- NSAIDs for symptoms of pain and inflammation
- Beta blockers for the symptoms of hyperthyroidism
- Levothyroxine for the symptoms of hypothyroidism
A small number (under 10%) remain hypothyroid long-term.
Thyroid Storm
Thyroid storm is a rare presentation of hyperthyroidism. It is also known as thyrotoxic crisis. It is a rare and more severe presentation of hyperthyroidism with fever, tachycardia and delirium. It can be life-threatening and requires admission for monitoring. It is treated the same way as any other presentation of thyrotoxicosis, although they may need additional supportive care with fluid resuscitation, anti-arrhythmic medication and beta blockers.
Management
A specialist endocrinologist guides the treatment of hyperthyroidism.
Carbimazole is the first-line anti-thyroid drug, usually taken for 12 to 18 months. Once the patient has normal thyroid hormone levels (usually within 4-8 weeks), they continue on maintenance carbimazole and either:
- The carbimazole dose is titrated to maintain normal levels (known as titration-block)
- A higher dose blocks all production, and levothyroxine is added and titrated to effect (known as block and replace)
TOM TIP: The MHRA issued a warning in 2019 about the risk of acute pancreatitis in patients taking carbimazole. In your exams, look out for a patient on carbimazole presenting with symptoms of pancreatitis (e.g., severe epigastric pain radiating to the back).
Propylthiouracil is the second-line anti-thyroid drug. It is used in a similar way to carbimazole. There is a small risk of severe liver reactions, including death, which is why carbimazole is preferred.
TOM TIP: Both carbimazole and propylthiouracil can cause agranulocytosis, with a dangerously low white blood cell counts. Agranulocytosis makes patients vulnerable to severe infections. A sore throat is a key presenting feature of agranulocytosis. In your exams, if you see a patient with a sore throat on carbimazole or propylthiouracil, the cause is likely agranulocytosis. They need an urgent full blood count and aggressive treatment of any infections.
Radioactive iodine treatment involves drinking a single dose of radioactive iodine. The thyroid gland takes this up, and the emitted radiation destroys a proportion of the thyroid cells. The reduction in the number of cells results in a decrease in thyroid hormone production. Remission can take 6 months, after which the thyroid is often underactive, requiring long-term levothyroxine. Treatment with radioactive iodine involves strict rules:
- Women must not be pregnant or breastfeeding and must not get pregnant within 6 months of treatment
- Men must not father children within 4 months of treatment
- Limit contact with people after the dose, particularly children and pregnant women
Beta blockers are used to block the adrenalin-related symptoms of hyperthyroidism. Propranolol is the usual choice, as it non-selectively blocks adrenergic activity (as opposed to something like bisoprolol, which is more selective). Beta blockers do not treat the underlying problem but control the symptoms, while definitive treatment takes time. They are particularly useful in patients with thyroid storm.
Surgery is a definitive option. Removing the whole thyroid gland (thyroidectomy), or the toxic nodules, effectively stops the excess thyroid hormone production. Patients will be hypothyroid after a thyroidectomy, requiring life-long levothyroxine.
Last updated March 2023
